A few months ago, I linked to Dr. Josh Farkas’ Internet Book Of Critical Care [Link is to the IBCC Table Of Contents] chapter & cast, “Approach to new fever or rigors in the ICU patient” [Link to the podcast] [Link to the show notes], by
Note to myself: I’m redoing the post (excerpting from it) today because I just rereviewed Dr. Farkas’ fever resources above. However, I remind myself that I do excerpting only because it helps me fix the material in my mind.
When I review the material I need to use the complete chapter notes on Dr. Farkas IBCC.
For my learning reinforcement, here are the excerpts:
CONTENTS [Each link below links directly to that section of the Chapter notes.]
- Definition & classification of fever
- Common causes of fever
- Evaluation
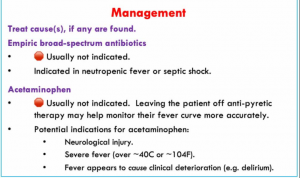
- Management
- Specific fever types
- Summary box
- Podcast
- Questions & discussion
- Pitfalls
- PDF of this chapter (or create customized PDF)
definition of a fever
- Fever is a bedrock concept in medicine, yet its precise definition remains a bit elusive.
- The Infectious Disease Society of America defined fever in the ICU as a temperature above 38.3/101.(18379262) This is generally a useful rule of thumb. However, a lower threshold for fever (>38/100.4) may be appropriate in some patients:
- Immunocompromised patients (e.g. neutropenic)
- Elderly patients
- Patients on scheduled acetaminophen or NSAIDs
- Precise temperatures may vary, depending on the site and the technique of measurement. Ideally, core temperature should be measured (e.g., rectal or esophageal temperature). However, in practice this is not routinely performed.
definition of ICU-acquired fever?
- This chapter explores new-onset fevers which occur after a couple days in the ICU, suggesting that the fever results from a process acquired within the hospital. For patients who develop fevers shortly after ICU admission, the differential diagnosis will be broader (with a greater focus on community-acquired infection).
- ICU-acquired fever should ideally be better defined. Based on definitions of ventilator-associated pneumonia, a fever arising >48 hours after hospital admission might be more likely to have been acquired within the hospital.
recognition of neutropenic fever
- Neutropenia is defined as absolute neutrophil count <500, or between 500-1000 and falling.
- Absolute neutrophil count = (WBC)(% bands + % neutrophils).
- 🧮 MDCalc calculator for absolute neutrophil count.
- Fever in the context of neutropenia is defined as a temperature above >38/100.4 for an hour, or a single measurement above 38.3/101.
- Neutropenic fever is critical to recognize, because these patients require empiric broad-spectrum antibiotics.
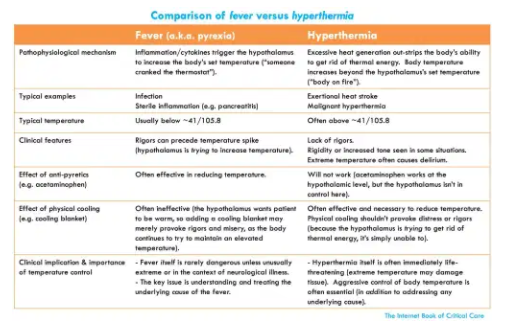
recognition of hyperthermia
- Hyperthermia is defined as elevated temperature resulting from extreme heat generation, rather than from an alteration of the hypothalamic set point.
- Hyperthermia is suggested by the following clinical features:
- Extreme temperature elevation (temperatures above roughly ~41/105.8).
- Skin may be hot and dry (but not always!).
- Antipyretics are ineffective.
- Hyperthermia has its own differential diagnosis and requires specific treatment.
- More on the critical distinction between fever versus hyperthermia:
appreciation of spontaneous rigors as a fever-equivalent
- Rigors are shaking chills, which which can be very dramatic. They represent an aggressive attempt by the hypothalamus to rapidly increase body temperature. A rigor will often precede development of a fever.
- Rigors are closely linked to bacteremia.(24298435) Although not supported by evidence specific to the ICU environment, it’s logical to investigate a patient with new-onset rigors in the same fashion as a patient with new-onset fever. Overall, evidence linking rigors to bacteremia is probably more persuasive than evidence linking fever to bacteremia.
common causes of fever in the ICU patient
infections (causing ~50% of fever in ICU)
- Pneumonia
- Clostridioides difficile
- Intravascular catheter infection
- Surgical site infection
- Urinary tract infection following the removal of a Foley catheter
- Metastatic or local complications from known infection (e.g., empyema, spinal abscess following endocarditis)
- Less often
- Acalculous cholecystitis
- Cellulitis, including infected decubitus ulceration
- Spontaneous bacterial peritonitis (SBP)
- 🦓 Urinary tract infection in a patient with a functioning Foley catheter (rare)
noninfectious
- Procedure-related
- Hemodialysis
- Bronchoscopy
- Febrile transfusion reaction (within 6 hours of transfusion)
- Benign post-operative fever (post-operative day #1-3)
- Medication-related
- Drug fever (more on this below).
- Medication-induced hyperthermia (serotonin syndrome, neuroleptic malignant syndrome, malignant hyperthermia)
- Sterile pulmonary inflammation (ARDS, aspiration pneumonitis)
- Pulmonary embolism (usually low-grade fever, <39/102).(10631196)
- Neurogenic fever (more on this below).
- Disorders which seldom arise in the ICU (yet may remain possible)
- 🦓 Pancreatitis
- 🦓 Thyroid storm or adrenal insufficiency
- 🦓 Rheumatologic disorders (vasculitis, gout flare)
- 🦓 Malignancy (especially lymphoma, hepatocellular carcinoma, renal cell carcinoma)
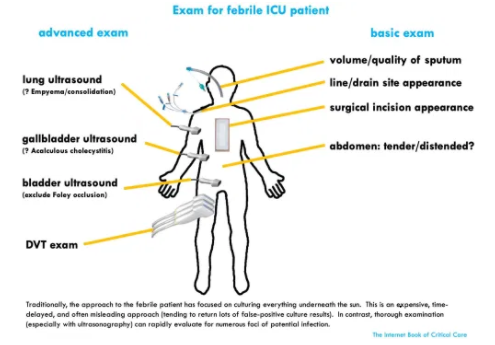
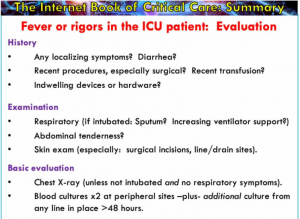
evaluation
[Please note that an abnormal abdominal physical examination or a fever of unknown origin may be an indication for CT scan of the Abdomen and Pelvis.]
basic evaluation
- Physical examination as above.
- Chest X-ray if the patient is intubated or has respiratory symptoms.
- Blood cultures:
- Two sets of peripheral blood cultures at different sites (each set contains an anaerobic bottle and an aerobic bottle).
- Additionally, any line in place >48-72 hours should be cultured.(18379262)
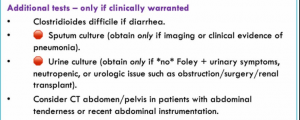
urine culture should usually be avoided 🛑
[See this section in the post for details.]
tracheal aspirate cultures should usually be avoided 🛑
[See this section in the post for details.]
other testing based on clinical scenario
- Clostridioides difficile testing is indicated for patients with diarrhea.
- Abdominal imaging is indicated for patients with abdominal pain or recent abdominal instrumentation. CT scan of the abdomen/pelvis is often most useful as a survey study, but right upper-quadrant ultrasonography may be useful if there is localizing pain in the right upper quadrant.
- If there are clinical features suggestive of venous thromboembolic disease, DVT ultrasonography or CT angiography of the chest may be warranted.
- Lumbar puncture is indicated if there is a reason to suspect meningitis (e.g., recent craniotomy or external ventricular drain). However, if an external ventricular drain is in place, fluid may be removed directly from the drain to avoid the risk of lumbar puncture.
- Paracentesis should be considered in the context of ascites, to exclude spontaneous bacterial peritonitis (SBP).
summary box