In this post, I link to and excerpt from Scientific Advances in and Clinical Approaches to Small-Fiber Polyneuropathy: A Review [PubMed Abstract] [Full-Text HTML] [Full-Text PDF]. Anne Louise Oaklander 1 2, Maria Nolano 3 4. JAMA Neurol. 2019 Oct 1;76(10):1240-1251. doi: 10.1001/jamaneurol.2019.2917.
Links to 93 similar articles in PubMed Central
The above article has been cited by 30 articles [Links]
All that follows is from the above resource.
Abstract
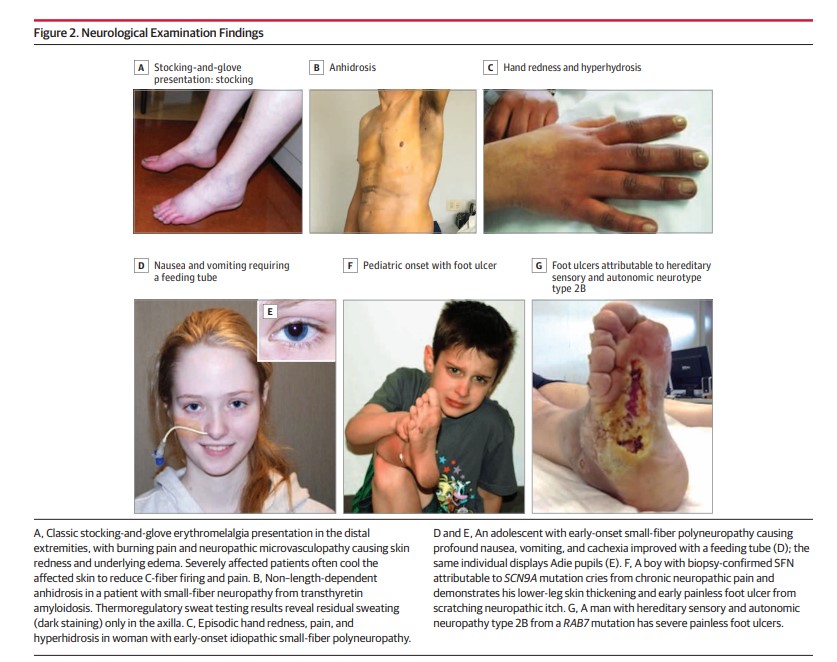
Importance: Small-fiber polyneuropathy involves preferential damage to the thinly myelinated A-delta fibers, unmyelinated C sensory fibers, or autonomic or trophic fibers. Although this condition is common, most patients still remain undiagnosed and untreated because of lagging medical and public awareness of research advances. Chronic bilateral neuropathic pain, fatigue, and nausea are cardinal symptoms that can cause disability and dependence, including pain medication dependence.
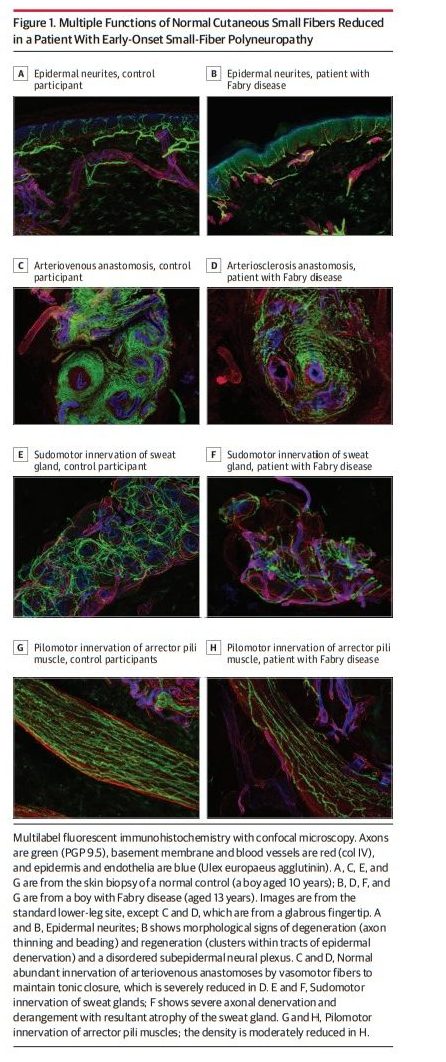
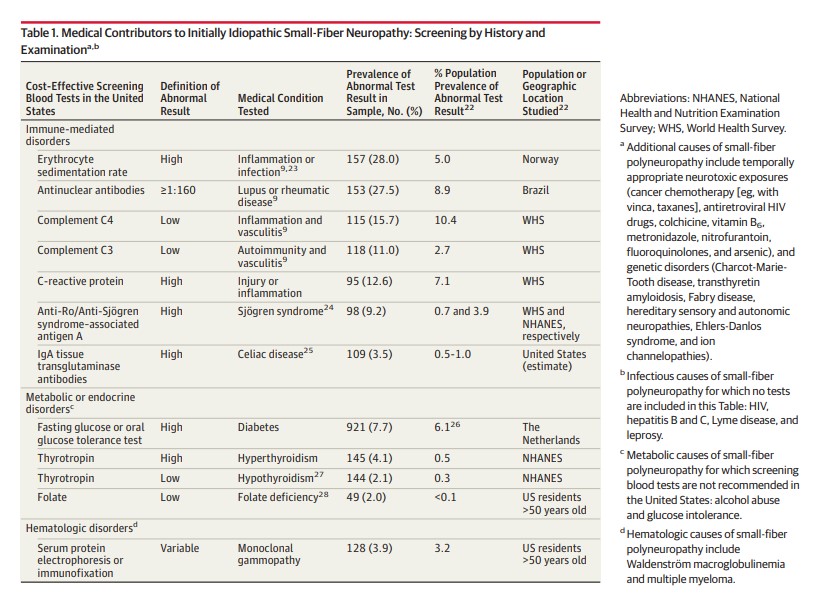
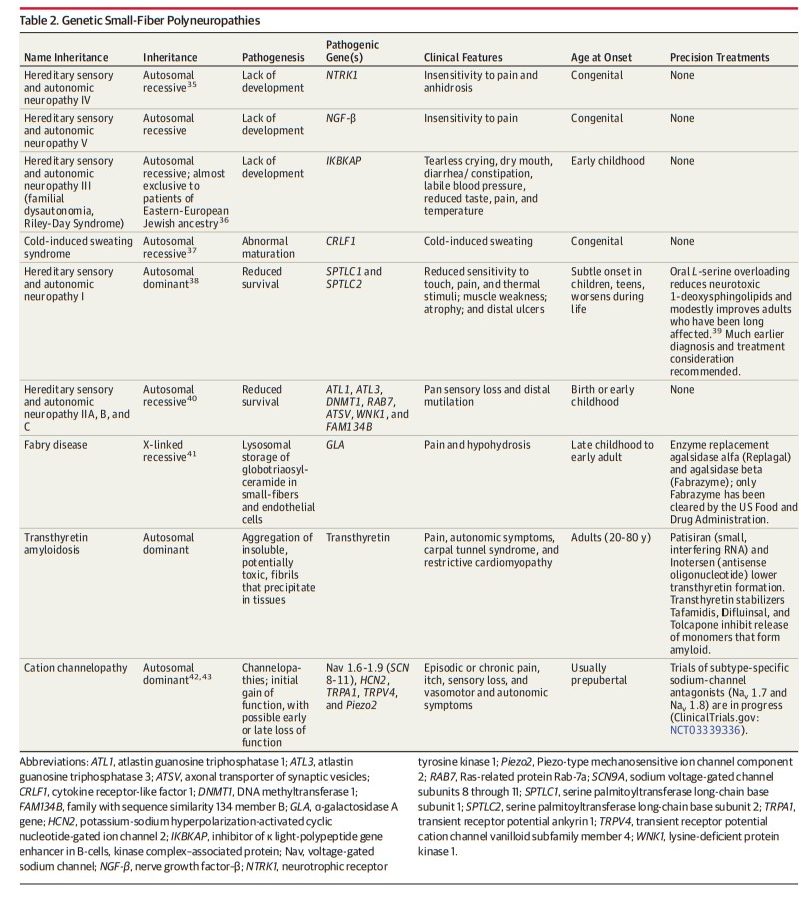
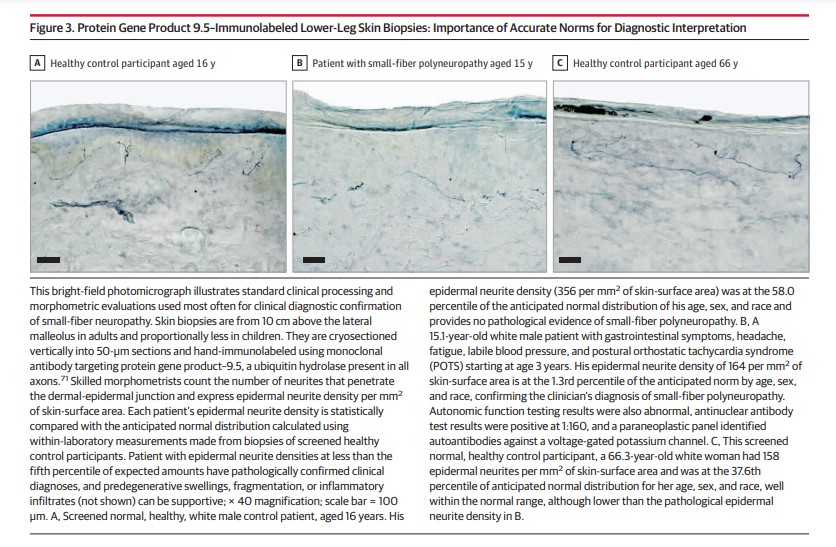
Observations: Biomarker confirmation is recommended, given the nonspecificity of symptoms. The standard test involves measuring epidermal neurite density within a 3-mm protein gene product 9.5 (PGP9.5)-immunolabeled lower-leg skin biopsy. Biopsies and autonomic function testing confirm that small-fiber neuropathy not uncommonly affects otherwise healthy children and young adults, in whom it is often associated with inflammation or dysimmunity. A recent meta-analysis concluded that small-fiber neuropathy underlies 49% of illnesses labeled as fibromyalgia. Initially, patients with idiopathic small-fiber disorders should be screened by medical history and blood tests for potentially treatable causes, which are identifiable in one-third to one-half of patients. Then, secondary genetic testing is particularly important for familial and childhood cases. Treatable genetic causes include Fabry disease, transthyretin and primary systemic amyloidosis, hereditary sensory autonomic neuropathy-1, and ion-channel mutations. Immunohistopathologic evidence suggests that small-fiber dysfunction and denervation, especially of blood vessels, contributes to diverse symptoms, including postexertional malaise, postural orthostatic tachycardia, and functional gastrointestinal distress. Preliminary evidence implicates acute or chronic autoreactivity in some cases, particularly in female patients and otherwise healthy children and young adults. Different temporal patterns akin to Guillain-Barré syndrome and chronic inflammatory demyelinating polyneuropathy have been described; here, corticosteroids and immunoglobulins, which are often efficacious for inflammatory neuropathic conditions, are increasingly considered.
Conclusions and relevance: Because small fibers normally grow throughout life, improving contributory conditions may permit regrowth, slow progression, and prevent permanent damage. The prognosis is often hopeful for improving quality of life and sometimes for abatement or resolution, particularly in the young and otherwise healthy individuals. Examples include diabetic, infectious, toxic, genetic, and inflammatory causes. The current standard of care requires prompt diagnosis and treatment, particularly in children and young adults, to restore life trajectory. Consensus diagnostic and tracking metrics should be established to facilitate treatment trials.