The following are excerpts from Reference (1), Validation of the “Step-by-Step” Approach in the Management of Young Febrile Infants, published in August 2016 in Pediatrics:
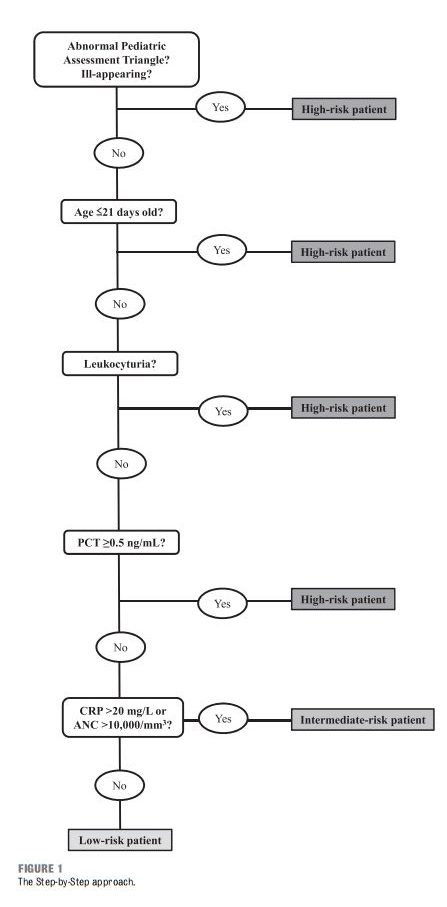
BACKGROUND: A sequential approach to young febrile infants on the basis of clinical and abstract
laboratory parameters, including procalcitonin, was recently described as an accurate
tool in identifying patients at risk for invasive bacterial infection (IBI). Our aim was to prospectively validate the Step-by-Step approach and compare it with the Rochester criteria and the Lab-score.
METHODS: Prospective study including infants ≤90 days with fever without source presenting in 11 European pediatric emergency departments between September 2012 and August
2014. The accuracy of the Step-by-Step approach, the Rochester criteria, and the Lab-score in identifying patients at low risk of IBI (isolation of a bacterial pathogen in a blood or
cerebrospinal fluid culture) was compared.
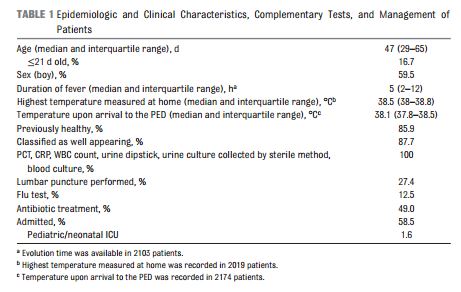
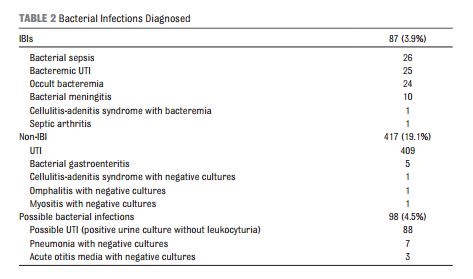
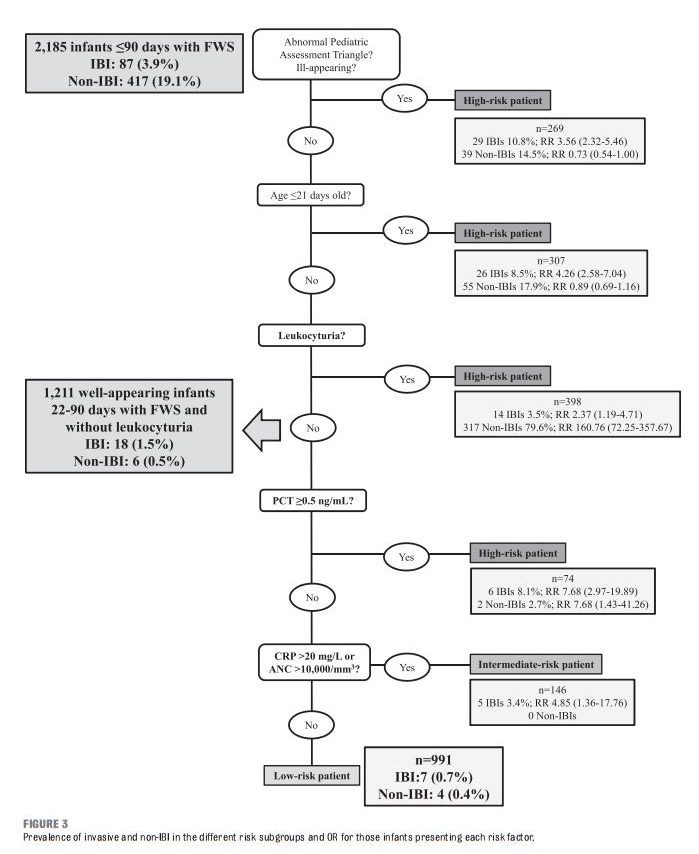
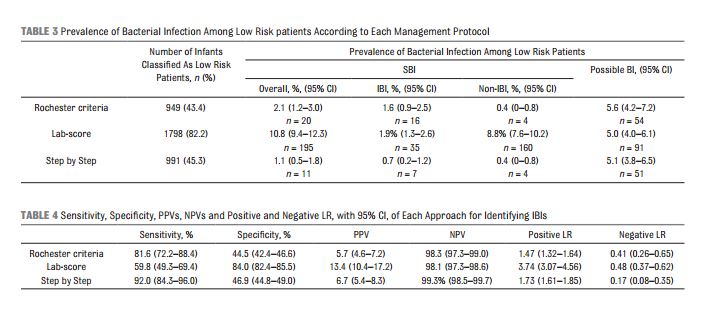
RESULTS: Eighty-seven of 2185 infants (4.0%) were diagnosed with an IBI. The prevalence of IBI was significantly higher in infants classified as high risk or intermediate risk according
to the Step by Step than in low risk patients. Sensitivity and negative predictive value for ruling out an IBI were 92.0% and 99.3% for the Step by Step, 81.6% and 98.3% for the Rochester criteria, and 59.8% and 98.1% for the Lab-score. Seven infants with an IBI were misclassified by the Step by Step, 16 by Rochester criteria, and 35 by the Lab-score.
CONCLUSIONS: We validated the Step by Step as a valuable tool for the management of infants with fever without source in the emergency department and confirmed its superior accuracy in identifying patients at low risk of IBI, compared with the Rochester criteria and the Lab-score.
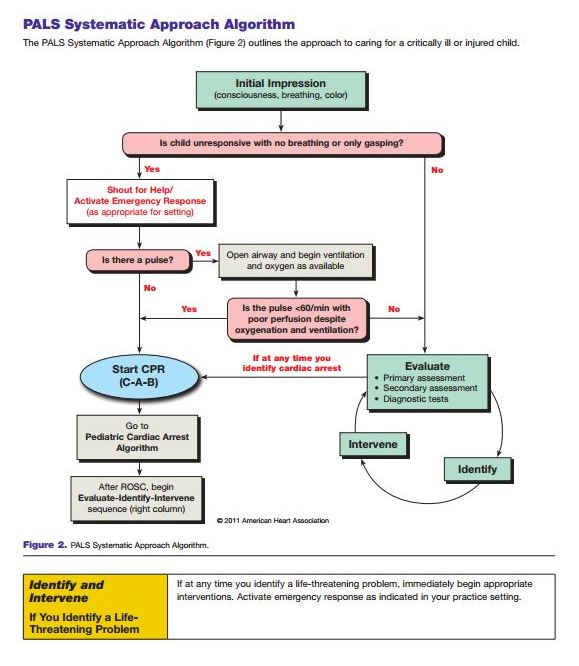
[The 2010 Pediatric Advanced Life Support Manual modified the Pediatric Assessment Triangle of the 2006 Pediatric Advanced Life Support Manual and it is now called the Initial Assessment – See the post The Initial Assessment–Formerly Called Pediatric Assessment Triangle posted on June 15, 2014 by Tom Wade MD. Reference (2). The Initial Assessment flow chart follows Reference (2) in Resources. So consult the Initial Assessment Flow Chart in Reference (2) or the Pediatric Assessment Triangle of Reference (3).]
DISCUSSION Our results validate the Step-byStep approach as an accurate tool to identify subgroups of young infants with FWS at different risk of IBI.
This approach includes both clinical and laboratory criteria, applying them in a sequential order, according to their clinical relevance, starting with the general appearance. Several studies have demonstrated that, as expected, febrile children who are not well appearing are at higher risk of bacterial infections, both in the general pediatric population 16 and in infants younger than 3 months. 17 In fact, clinical appearance is the factor that mostly increases this risk. 16, 17
Infants 21 to 28 days old had a similar prevalence of bacterial infections compared with older patients and a lower rate than infants ≤21 days old.
[The article urges caution, however, in using the 21 day cutoff ] Of note, in our study, 4 of the 7 patients finally diagnosed with an IBI and classified by the Step by Step as low risk patients were 22 to 28 days old (Supplemental Table 7). This finding, not observed in our previous retrospective study, 11 suggests to be cautious when assessing patients in the fourth week of age and recommends further studies to safely identify the best secondary age cutoff point.
Finally, leukocyturia identifies those infants with a high probability of having a UTI but also a subgroup of infants with an increased risk of having a bacteremia. 17 Indeed 1 of the most frequent IBI in young febrile infants is UTI with associated bacteremia. 23, 24
In our study, general appearance, age, and urine dipstick identified almost 80% of the IBI patients and, more interestingly, 85% of the sepsis and 90% of the bacterial meningitis. The bacterial meningitis and 3 of the 4 bacterial sepsis not detected by this first part of the algorithm would have been identified by an elevated PCT value. Several studies have compared the performance of PCT and CRP in the management of young febrile infants. 25–27 PCT is a better biomarker to rule in an IBI, and, due its more rapid kinetic, 28 it is a more suitable biomarker in young infants who, for the great majority, present to the PED with a very early onset fever.17, 26, 27, 29 However, in 6 of 7 patients potentially missed by the Step by Step, fever duration was less than 2 hours, which is far too short even for PCT to rise. This very short fever duration makes the evaluation of these patients even more challenging and highlights the important role of a short-term PED observation in the management of these patients.
The intermediate risk group includes patients with an elevated CRP or ANC. We excluded the WBC count, because neither leukocytosis nor leukopenia have proved to be good predictors of bacterial infection in young infants. 30–33
CONCLUSIONS The Step-by-Step approach revealed a high sensitivity, being more accurate than the Rochester criteria and the Lab-score at identifying children at low risk of IBI, and appears to be a useful tool for the management of the febrile infant in the ED. However, as no perfect tool exists, the Step by Step is not 100% sensitive and physicians should use caution especially when assessing infants with very short fever evolution. For this subgroup of patients, we strongly advise for an initial period of close observation and monitoring in the ED, even when all the complementary test values are normal.
Resources:
(1) Validation of the “Step-by-Step” Approach in the Management of Young Febrile Infants [PubMed Abstracts] [Full Text HTML] [Full Text PDF]. Pediatrics. 2016 Aug;138(2). pii: e20154381. doi: 10.1542/peds.2015-4381. Epub 2016 Jul 5.
(2) The Initial Assessment–Formerly Called Pediatric Assessment Triangle posted on June 15, 2014 by Tom Wade MD. What follows below is the Initial Assessment Flow Chart:
(3) Pediatric Assessment Triangle 01/04 from the New York State Emergency Services.
(2) STEP BY STEP – A NEW APPROACH TO FEBRILE INFANTS by Dr. Henry Goldstein of the website Don’t Forget the Bubbles which is a paediatric blog providing online medical education. It “is run by Tessa Davis, Henry Goldstein, Ben Lawton and Andrew Tagg, and is a collaborative effort to create a Free Open Access Medical Education (FOAM) resource for paediatrics. We have no external funding and exclusively fund DFTB ourselves.”