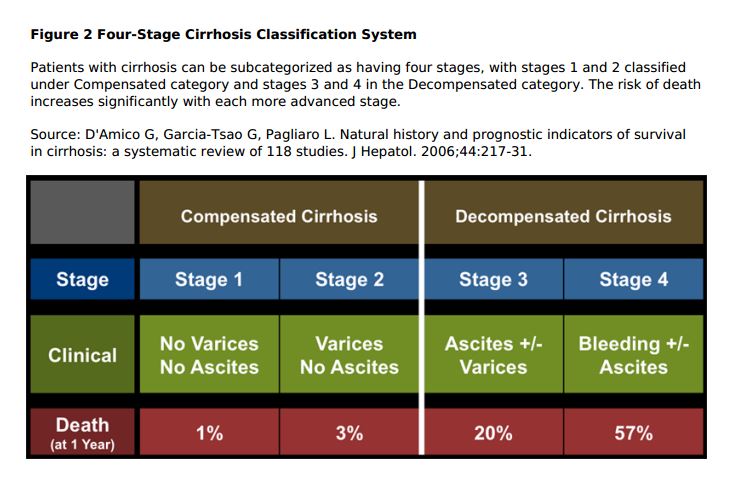
It is critical to determine whether the patient with cirrhosis has compensated cirrhosis or decompensated cirrhosis as the prognosis and monitoring of the two conditions is very different.
What follows is from Reference (1) in Resources:
Compensated Cirrhosis
Definition and Natural History: Cirrhosis is considered to be compensated in the asymptomatic patient with or without gastroesophageal varices. Compensated cirrhotics are not jaundiced and have not yet developed ascites, variceal bleeding, or hepatic encephalopathy. Cirrhosis can remain compensated for many years. The transition from compensated to decompensated cirrhosis occurs at a rate of approximately 5 to 7% per year. The median survival of compensated cirrhotics has been reported to be 9 to 12 years.
Management: The major goal of managing patients with HCV and compensated cirrhosis is to treat the HCV infection. Patients with HCV-related cirrhosis who undergo treatment and achieve a cure have a dramatically decreased 10-year risk of all-cause mortality (Hazard ratio [HR] = 0.26), liverrelated mortality or transplantation (HR = 0.06), hepatocellular carcinoma (HR = 0.19), and hepatic decompensation (HR = 0.07). In addition, all patients with cirrhosis should undergo surveillance for hepatocellular carcinoma with hepatic ultrasound every 6 months and they should have a screening endoscopy to determine whether they have gastroesophageal varices (and if present evaluation of the size of the varices).
Gastroesophageal Varices: Approximately 50% of persons with cirrhosis develop gastroesophageal varices. Screening for gastroesophageal varices with an upper endoscopy is an important preventive measure for all patients with cirrhosis. Patients found to have large varices or high-risk small varices should receive primary prophylaxis with either non-selective beta-blockers (NSBB) or endoscopic variceal ligation. Endoscopic variceal ligation is not recommended in patients with gastric varices. If no gastroesophageal varices are identified, the upper endoscopy should be repeated in 2 to 3 years.
Decompensated Cirrhosis
Definition and Natural History: Decompensated cirrhosis is defined by the development of jaundice, ascites, variceal hemorrhage, or hepatic encephalopathy. A MELD score should be calculated for all patients with decompensated to better estimate the survival probability. In general, survival is poor in patients with decompensated cirrhosis and they should be considered for liver transplantation. Patients with ascites and variceal hemorrhage have a reported 1-year survival rate of less than 50%. Hepatitis C treatment in patients with decompensated cirrhosis has become possible with new interferon-free all-oral regimens. Ascites: Ascites is the pathologic accumulation of fluid in the peritoneal cavity. It is the most common complication of cirrhosis. Following the development of ascites, a patient’s 1-year survival is only 50%. Ascites is caused by portal hypertension, which results in increased pressure within the splanchnic bed, and reduced protein production by the liver, which causes decreased oncotic pressure. Although treatment of ascites does not result in enhanced survival, it does improve the patient’s quality of life and decreases the risk of developing spontaneous bacterial peritonitis (SBP). Standard of care for the treatment of ascites involves sodium restriction and diuretic therapy with spironolactone alone or with furosemide.
Variceal Hemorrhage: The rate of bleeding with know varices is 12 to 15% per year. The mortality rate from each episode of variceal hemorrhage is approximately 15 to 20%. Acute variceal bleeding is a medical emergency and involves control of bleeding and prevention of complications. The risk of rebleeding within 1 to 2 years of the initial bleed is approximately 60%. It is extremely important that patients who survive an initial variceal hemorrhage start on prophylactic therapy to prevent future bleeds (see section above on Gastroesophageal Varices).
Hepatic Encephalopathy: Hepatic encephalopathy is thought to result from a buildup of toxic compounds generated by gut bacteria. These compounds are transported through the portal vein to the liver and metabolized and excreted immediately in a normal liver; in patients with cirrhosis, however, these toxins are not metabolized properly. Patients who develop hepatic encephalopathy may have subtle symptoms and the onset is often insidious. Hepatic encephalopathy represents a continuum from minimal to overt and can be episodic or persistent. The patient may have subtle and intermittent changes in personality, memory, concentration, and reaction time. Hepatic encephalopathy is a diagnosis of exclusion. The major goals of therapy include identification and correction of precipitating factors (such as infection and gastrointestinal hemorrhage) and reducing ammonia levels. Lactulose is the treatment of choice. It is a non-absorbable disaccharide that reduces ammonia by acidifying the colon and reducing colonic transit time.
Hepatorenal Syndrome: Hepatorenal syndrome is defined as renal failure in a patient with cirrhosis in the absence of intrinsic renal disease. The pathophysiology of hepatorenal syndrome is not completely understood, but it is thought to occur secondary to underfilling of the arterial circulation because of arterial vasodilation in the splanchnic circulation. This causes sodium and water retention in patients with renal vasoconstriction, which results in decreased renal blood flow and urinary output. Hepatorenal syndrome has been divided into 2 types: type 1 and type 2. Type 1 is rapidly progressive with a survival of approximately 2 weeks. The median survival for patients with Type 2 is 6 months.
Spontaneous Bacterial Peritonitis (SBP): SPB is the most common infection in patients with cirrhosis and ascites. SBP occurs in 10 to 20% of hospitalized patients with cirrhosis and in-hospital mortality for an episode of SPB is reported in the range of 10 to 20%. The recurrence rate of SBP after an initial episode is very high (approximately 70%). Patients who survive an initial episode of SBP should receive antibiotic prophylaxis.
Resources
(1) Evaluation and Prognosis of Patients with Cirrhosis, July 6, 2016, from Hepatitis C Online