I recently completed the International Trauma Life Support Course (ITLS) at IU Health Methodist Hospital in Indianapolis. It was an excellent course and I believe that any clinician interested in trauma care will benefit from it.
This blog is basically my study notes and my peripheral brain. Placing my notes online makes makes them available to me anywhere. And that is because the excellent built-in search function of the content management software [WordPress] makes it easy to find my notes on any topic when I want to review them.
This post contains excerpts from International Trauma Life Support For Emergency Care Providers Provider Manual, 2016*.
* Here are links to:
Specifically, this post consists of excerpts from Chapter 10 Head Trauma and Traumatic Brain Injury, 189 – 207.
Excerpts:
Chapter Overview
Head injury or, more specifically, traumatic brain injury (TBI), is a major cause of death and disability in multiple-trauma patients worldwide. Of all multiple-system trauma patients, 40% have a central nervous system (CNS) injury. Those patients
have a death rate twice as high (35% versus 17%) as that of patients with no CNS injuries. Traumatic brain injuries account for an estimated 25% of all trauma deaths and up to one-half of all motor-vehicle fatalities. Worldwide, the cost of TBI is staggering in terms of lives lost, families destroyed, and money spent for care. Prevention remains the most effective treatment. EMS personnel can help reduce this major epidemic by encouraging the use of helmets in sports and work and restraint devices in vehicles.As an emergency care provider, you may encounter head injuries that can range from the trivial to the immediately life threatening. By recognizing injuries that need immediate intervention and providing transport to the appropriate facility, you can significantly improve the chances for a patient to have a good outcome. Not every injury to the head results in a traumatic brain injury. Some may only involve the scalp, skull, or face. An injury above the clavicle should prompt the emergency care provider to look for TBI.
Because it is not possible to perform a field clearance of the cervical spine in a patient with altered mental status, you must always assume that a serious head injury is accompanied by an injury to the cervical spine and spinal cord and provide appropriate spinal motion restriction (SMR), as described elsewhere in this text. (See Chapter 12.)
Beginning with the third edition of this text, material included in this chapter has been based on the recommendations of the Brain Trauma Foundation (BTF; a multidisciplinary organization dedicated to improving care of TBI victims by use of evidence-based treatment).
Primary Brain Injury:
The immediate damage to the brain tissue that is the direct result of an injury force.
Secondary Brain Injury:
An injury to the brain that is the result
of hypoxia and/or decreased perfusion of brain tissue after a primary injury.PEARLS
Hypoxia and Hypotension
• Patients with serious head injuries cannot tolerate hypoxia or hypotension. Give high-flow oxygen and monitor oxygenation with a pulse oximeter.
• Pediatric patients usually have a better recovery from TBI. However, hypoxia and hypotension appear to eliminate any neuroprotective mechanism normally afforded by age. If the child with a serious brain injury is allowed to become hypoxic or hypotensive, the chance of recovery is even worse than an adult with the same injury.
Intracranial Pressure
Brain tissue, cerebrospinal fluid, and blood reside within the skull and fibrous coverings of the brain. An increase in the volume of any one of those components must
be at the expense of the other two because the adult skull (a rigid box) cannot expand. Although there is some displacement volume of cerebrospinal fluid and venous blood, it accounts for little space and cannot offset rapid brain swelling.
Blood supply will be decreased by increased ICP, and because the brain requires a constant supply of blood (oxygen and glucose) to survive, brain swelling can be rapidly catastrophic.The pressure of the brain and contents within the skull is termed intracranial pressure (ICP). ICP is considered dangerous when it rises above 15 mm Hg; cerebral herniation may occur at pressures above 25 mm Hg. The net pressure gradient causing blood flow through the brain is termed the cerebral perfusion pressure (CPP). Its value is obtained by subtracting the intracranial (intracerebral) pressure from the
mean arterial blood pressure (MAP).
MAP = Diastolic BP + 1/3 (Systolic BP − Diastolic BP)
CPP = MAP − ICPIf the brain swells or if bleeding occurs inside the skull, ICP increases, and the perfusion pressure decreases, resulting in cerebral ischemia (hypoxia). If the swelling of the brain is severe enough, the ICP equals the MAP, and blood flow to the brain ceases. In the late stage, hypertension, bradycardia, and irregular respiration known as Cushing’s reflex occurs, which is associated with markedly elevated ICP and herniation. When the ICP increases, the systemic blood pressure increases to try to preserve blood flow to the brain. The body senses the rise in systemic blood pressure, and this triggers a drop in the pulse rate as the body tries to lower the systemic blood pressure. With severe injury or ischemia, the pressure within the skull continues in an upward spiral until a critical point at which the ICP approaches the MAP, and there is no cerebral perfusion. All
vital signs deteriorate, and the patient dies. Because CPP depends on both the arterial pressure and the ICP, hypotension also will have a devastating effect if the ICP is high.As stated earlier, the injured brain loses the ability to autoregulate blood flow. In this situation perfusion of the brain is directly dependent on arterial blood pressure. You must maintain a CPP of at least 60 mm Hg (see earlier formula), which requires maintaining a systolic blood pressure of at least 100 mm Hg in the patient with TBI. Hypotension due to TBI is rare, occurring in about 5% of patients with isolated severe TBI (GCS of < 9). A patient with a significant TBI who is hypotensive is bleeding from somewhere or has a cord injury causing spinal shock. Stopping the hemorrhage and restoring perfusion is important. Overly aggressive attempts to maintain CPP above 70 mm Hg with fluids may lead to the development of the adult respiratory distress syndrome (ARDS). However, this does not happen immediately. Pressors such as dopamine may also be helpful in maintaining perfusion. Remember, hypotension and the associated poor perfusion is devastating to the injured brain.
Cerebral Herniation Syndrome
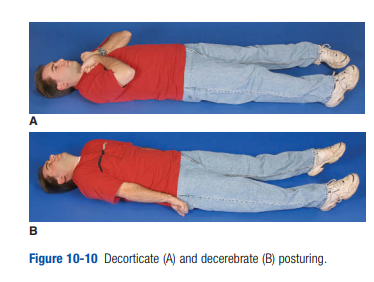
The classic findings of this life-threatening situation are a
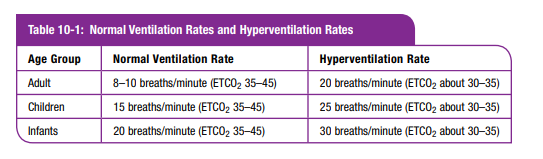
decreasing level of consciousness (LOC) that rapidly progresses to coma, dilation of the pupil and an outward–downward deviation of the eye on the side of the injury, paralysis of the arm and leg on the side opposite the injury, or decerebrate posturing (arms and legs extended). As the cerebral herniation is occurring, the vital signs frequently reveal increased blood pressure and bradycardia (Cushing’s reflex). The patient may soon cease all movement, stop breathing, and die. This syndrome often follows an acute epidural or subdural hemorrhage.If these signs are developing in a TBI patient, cerebral herniation is imminent, and aggressive therapy is needed. As noted earlier, hyperventilation will decrease the size of the blood vessels in the brain and briefly decrease ICP. In this situation the danger of immediate herniation outweighs the risk of cerebral ischemia that can follow hyperventilation. The cerebral herniation syndrome is the only situation in which hyperventilation is still indicated. (You must ventilate every three seconds [20/minute] for adults, every two and one-half seconds [25/minute] for children older than one year, and every two seconds [30/minute] for infants younger than one year.) If you have waveform capnography, attempt to keep the ETCO2 at about 30 to 35 mm Hg.
To simplify knowing when to hyperventilate in the field, the clinical signs of cerebral herniation in the patient who has had hypoxemia and hypotension corrected are any one (or more) of the following:
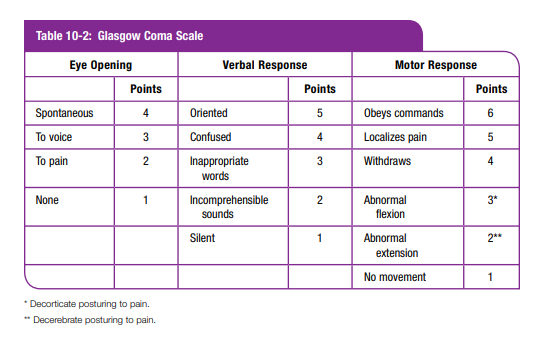
• TBI patient with a Glasgow Coma Scale (GCS) score < 9 with extensor posturing (decerebrate posturing)
• TBI patient with a GCS score < 9 with asymmetric (or bilateral), dilated, or nonreactive pupils
• TBI patient with an initial GCS score < 9, who then drops his or her GCS by more than two pointsFor the preceding, “asymmetric pupils” means 1 mm (or more) difference in the size of one pupil, “fixed” means no response (<1 mm) to bright light. Bilateral dilated and fixed pupils usually are a sign of brainstem injury and are associated with greater
than 90% mortality. A unilateral dilated and fixed pupil has been associated with good recovery in up to 54% of patients. Remember that hypoxemia, orbital trauma, drugs, lightning strike, and hypothermia also affect pupillary reaction, so take this into account before beginning hyperventilation. Flaccid paralysis usually means spinal-cord injury. If the patient has signs of herniation (as listed earlier) and the signs resolve with hyperventilation, you should discontinue the hyperventilation.
(See Table 10-1.)
PEARLS
Altered Mental Status
Remember that hypoglycemia, hypoxia, cardiac dysrhythmias, and drugs can cause altered mental status. When narcotic abuse is a possibility, administer naloxone (Narcan®) to any patient with altered mental status. Monitor the heart and oxygenation, and check the blood glucose level on all patients with altered mental status. If you cannot perform a glucose determination but suspect hypoglycemia (diabetics and alcoholics), give glucose or thiamine and glucose.
Evaluation of the Traumatic Brain
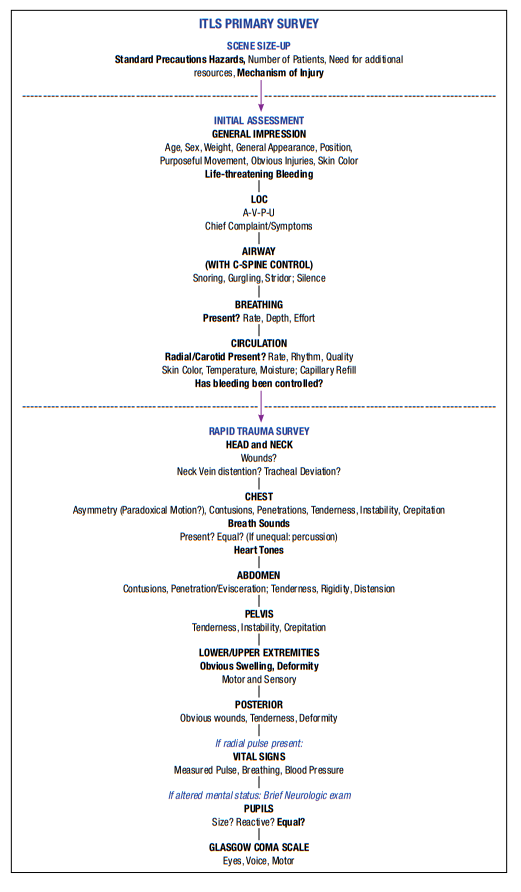
Injury PatientITLS Primary Primary Survey
Remember that every trauma patient is initially evaluated in the same sequence (Figure 10-7).
Figure 10-7 The ITLS Primary Survey:
Scene Size-up
The results of the scene size-up will begin to determine if you have a load-and-go patient*.
*Chapter 2 pp 40 +41 Critical Interventions and Transport Decisions:
When you have completed the initial assessment and rapid trauma survey or focused exam, enough information is available to decide if a critical situation is
present. Patients with critical trauma situations are transported immediately. Most treatment interventions will be done during transport.If your patient has any of the following critical injuries or conditions, transport immediately.
• Initial assessment reveals:
—Altered mental status
—Abnormal breathing
—Abnormal circulation (shock or uncontrolled bleeding)• Signs discovered during the rapid trauma survey of conditions that can rapidly lead
to shock:
—Penetrating wounds of the torso
—Abnormal chest exam (flail chest, open wound, tension pneumothorax, hemothorax)
—Tender, distended abdomen
—Pelvic instability
—Bilateral femur fractures
- Significant mechanism of injury and/or poor general health of patient. Even though the
patient appears to be stable, if there is a dangerous mechanism or other dangers
(such as age, poor general health, death of another passenger in the same auto), consider early transport. “Stable” patients can become unstable quite rapidly.If the patient has one of the critical conditions listed, after the rapid trauma survey or focused exam, immediately load the patient into an ambulance and transport rapidly to the nearest appropriate emergency facility. When in doubt, transport early.
The following procedures are done at the scene, and most of them can be delegated to team members to perform while you continue the ITLS Primary Survey: control major external bleeding, open and maintain a patent airway (position, sweep, suction; intubate if indicated and necessary), ventilate, apply oxygen, CP, seal sucking chest wounds, stabilize flail segments, decompress tension pneumothorax when indicated, stabilize penetrating objects, and maintain SMR if indicated.
Procedures that are not life saving, such as splinting, bandaging, insertion of IV lines,
or even elective endotracheal intubation, must not hold up transport of the critical patient. At this point, the ITLS Primary Survey is over, and the team leader may help
the other emergency care providers with patient care.
I’m now returning to excerpts from Chapter 10:
Initial Assessment
start here p 199