In Resources I have placed links to two useful guidelines on cirrhosis with ascites.
What follows is from Reference (1):
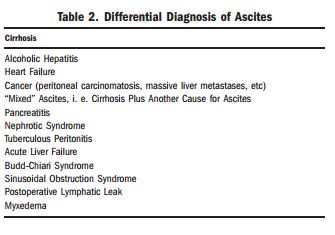
Most patients (approximately 85%) with
ascites in the United States have cirrhosis (Table 2).10
In about 15% of patients with ascites, there is a nonhepatic
cause of fluid retention. Successful treatment is
dependent on an accurate diagnosis of the cause of ascites;
e.g., peritoneal carcinomatosis does not respond
to diuretic therapy. Patients with ascites should be
questioned about risk factors for liver disease. Those
who lack an apparent cause for cirrhosis should also be
questioned about lifetime body weight (to determine
the number of years of overweight or obesity) and diabetes
as nonalcoholic steatohepatitis has been concluded
to be causative in many of these patients.11
Past history of cancer, heart failure, renal disease, thyroid
disease or tuberculosis is also relevant. Hemophagocytic
syndrome can masquerade as cirrhosis with ascites.12
These patients have fever, jaundice, and
hepatosplenomegaly, usually in the setting of lymphoma
or leukemia.12The physical examination for detecting ascites in the
obese patient is problematic. An abdominal ultrasound
may be required to determine with certainty if fluid is
present. Ascites usually is present for only a few weeks
before the patient seeks medical attention. In contrast
a slowly enlarging abdomen over months to years is
most likely due to obesity not ascites.
The diagnosis of new-onset ascites is suspected on
the basis of the history and physical examination and
usually confirmed by successful abdominal paracentesis
and/or ultrasound. The diagnosis of the etiology of ascites
formation is based on the results of the history,
physical, and ascitic fluid analysis. In general, few
other tests are required. However, the liver is commonly
imaged to screen for morphologic evidence of
cirrhosis and portal hypertension, tumors, portal vein
thrombosis, and hepatic vein thrombosis.Abdominal paracentesis with appropriate ascitic fluid analysis is probably the most rapid and cost-effective method of diagnosing the cause of ascites.16,17 Fluid due to portal hypertension can be readily differentiated from fluid due to
other causes.10 Also, in view of the high prevalence of
ascitic fluid infection at the time of admission to the
hospital, an admission surveillance tap may detect
unexpected infection.18
Resources:
(8) Management of Adult Patients with Ascites Due to Cirrhosis: Update 2012 [Full Text PDF] from The American Association For The Study Of Liver Diseases
(2) EASL clinical practice guidelines on the management of ascites, spontaneous bacterial peritonitis, and hepatorenal syndrome in cirrhosis [PubMed Citation] [Full Text HTML] [Full Text PDF] European Association for the Study of the Liver.
J Hepatol. 2010 Sep;53(3):397-417. doi: 10.1016/j.jhep.2010.05.004. Epub 2010 Jun 1.