In this post I link to and excerpt from Kids Really Are Just Small Adults: Utilizing the Pediatric Triangle with the Classic ABCD Approach to Assess Pediatric Patients [PubMed Abstract] [Full Text HTML] [Full Text PDF]. Cureus. 2020 Mar; 12(3): e7424.
Here are excerpts:
Abstract
Pediatric altered mental status is a commonly feared presentation of children in both the emergency department and prehospital setting. Given the usual difficulties we face when
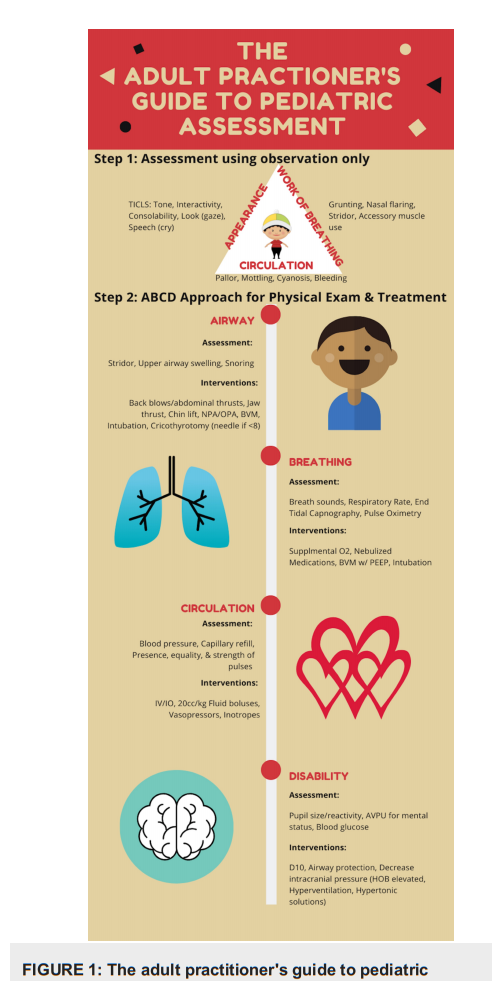
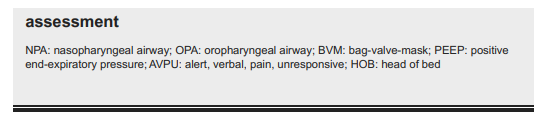
treating children, utilizing systematic tools can help us to remain thorough and consistent when evaluating any given child. By using a standardized method of evaluation and diagnosis, first responders and emergency physicians can set aside their worries of mismanagement and provide adequate care to children with undifferentiated altered mental status. This article reviews one of the many approaches toward assessing children’s clinical status, walks through the elements that comprise it, and examines how it can be used to make emergency providers more confident.Each side of the Pediatric Assessment Triangle represents an area of assessment: appearance, work of breathing, and circulation. Many utilize the triangle simply to remember these key areas. Taken a step further, if we shade in the side(s) of the triangle with the abnormal findings, we can create a table that gives a differential (Table 1).
The differentials are broad and include the following parameters: stable, respiratory distress, respiratory failure, shock, central nervous system/metabolic issues, and cardiopulmonary failure. As an example, if the child only has an issue with work of breathing, the chart points us to respiratory distress, whereas if there is an issue with work of breathing and appearance, it is likely to be respiratory failure.
There are many similarities between the adult and pediatric assessment with regard to two of the three categories in the Pediatric Assessment Triangle: work of breathing and circulation.
However, appearance is very specific to pediatrics. For this reason, it is helpful to remember the mnemonic TICLS. It stands for tone, interactivity, consolability, look (gaze), and speech (cry). When it comes to assessing the appearance of the child, it becomes important to observe their tone. We will ask ourselves, “are they limp or are they stiff?” We will also be observing their interaction with their caregivers. Do they make eye contact? Are they tracking? Are they consolable? Lastly, for appearance, we are listening for the pitch of their cry and, if they are old enough to speak, we are observing their speech patterns.
After determining whether the child is sick, which will help us in determining what resources we need to mobilize, the ABCD approach can be used to further assess the child. This will now
incorporate physical exam findings, objective measurements, and life-saving treatments. What is helpful about the ABCD approach is that it is generalizable to both adults and pediatrics.
Noticing the similarities decreases the stress level and the need for reliance on memorization.
Be sure to review the ABCD steps detailed in the article.
Conclussions
When dealing with sick children, it is important to have a systematic approach with as little memorization as possible. For those taking care of both adults and kids, merging these two assessments into one will help to retain as much information as possible. We usually talk about how kids are not just small adults, but often we do not highlight the similarities.
Highlighting the similarities will allow us to simplify the overall clinical assessment approach and help us to categorize sick vs. not sick, which is the first step in the practice of emergency medicine.