It is important to remember that the majority of patients with sexually transmitted diseases are asymptomatic.
Therefore, taking a sexual history can be very important. Please see my post How To Take A Sexual History – Help From The Centers For Disease Control And Prevention (CDC)
Posted on November 29, 2018 by Tom Wade MD.
The above post contains a script from the CDC that you can use to take your sexual history.
What follows are resources from the CDC on when and how to test for Hepatitis B and Hepatitis C infection.
Please see also my post on Dx And Rx Of STDs – Help From The Curbsiders.
Testing and Public Health Management of Persons with Chronic Hepatitis B Virus Infection:
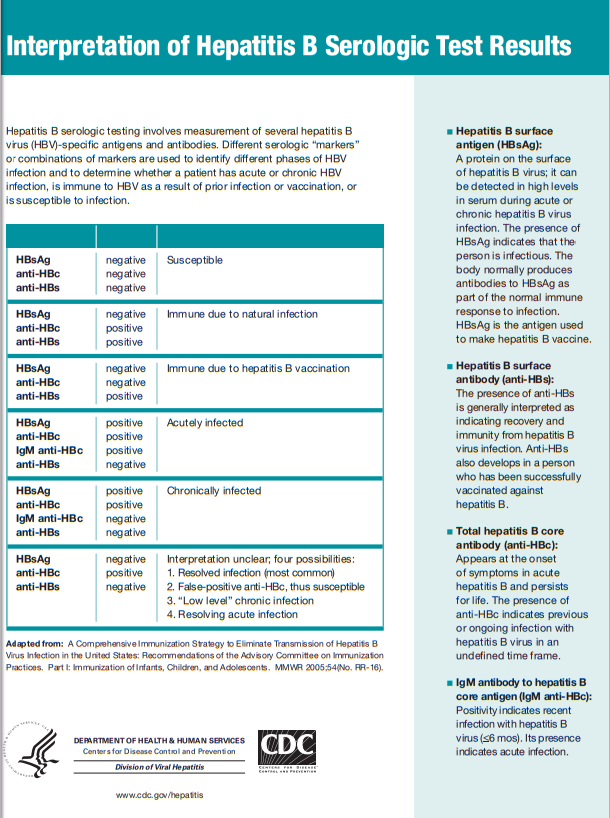
On September 19, 2008, CDC published updated and expanded guidelines for testing for chronic Hepatitis B virus (HBV) infection and recommendations for public health evaluation and management for chronically infected persons and their contacts. Serologic testing for Hepatitis B surface antigen (HBsAg) is the primary way to identify persons chronic HBV infection.
Testing for HBsAg now is recommended for:
- persons born in geographic regions with HBsAg prevalence of ≥2%
- US born persons not vaccinated as infants whose parents were born in geographic regions with HBsAg prevalence of ≥8%
- injection-drug users
- men who have sex with men
- persons with elevated ALT/AST of unknown etiology
- persons with selected medical conditions who require immunosuppressive therapy
Testing continues to be recommended for:
- pregnant women
- infants born to HBsAg-positive mothers
- household contacts and sex partners of HBV-infected persons
- persons who are the source of blood or body fluid exposures that might warrant postexposure prophylaxis (e.g., needlestick injury to a health care worker)
- persons infected with HIV
Testing Recommendations for Hepatitis C Virus Infection
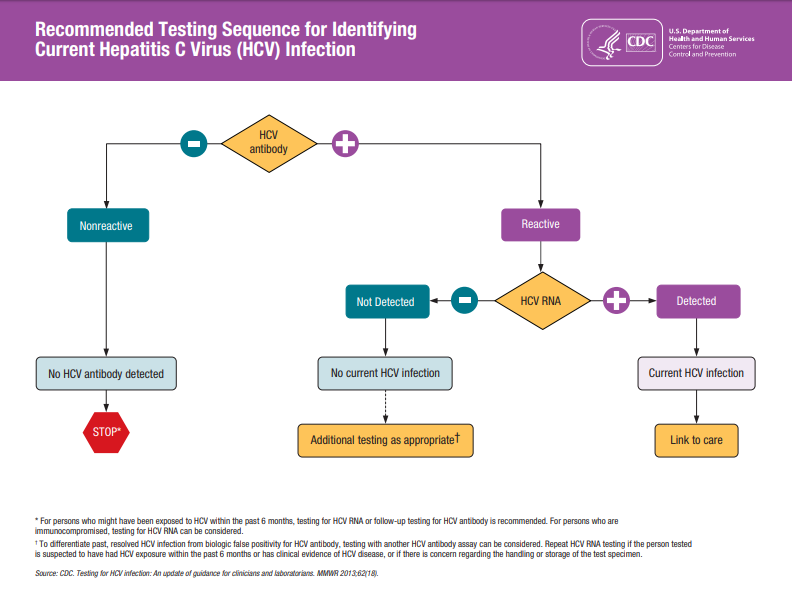
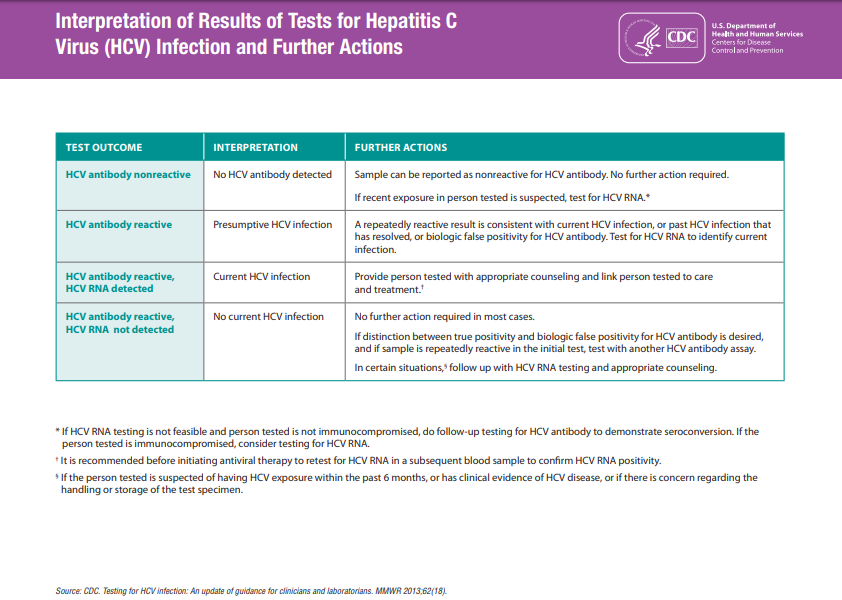
CDC’s Testing Recommendations for hepatitis C virus infection are outlined below. Testing should be initiated with anti-HCV. For those with reactive test results, the anti-HCV test should be followed with an HCV RNA.
Persons for Whom HCV Testing Is Recommended
- Adults born from 1945 through 1965 should be tested once (without prior ascertainment of HCV risk factors)
- HCV testing is recommended for those who:
- Currently injecting drugs
- Ever injected drugs, including those who injected once or a few times many years ago
- Have certain medical conditions, including persons:
- who received clotting factor concentrates produced before 1987
- who were ever on long-term hemodialysis
- with persistently abnormal alanine aminotransferase levels (ALT)
- who have HIV infection
- Were prior recipients of transfusions or organ transplants, including persons who:
- were notified that they received blood from a donor who later tested positive for HCV infection
- received a transfusion of blood, blood components, or an organ transplant before July 1992
- HCV- testing based on a recognized exposure is recommended for:
- Healthcare, emergency medical, and public safety workers after needle sticks, sharps, or mucosal exposures to HCV-positive blood
- Children born to HCV-positive women
Note: For persons who might have been exposed to HCV within the past 6 months, testing for HCV RNA or follow-up testing for HCV antibody is recommended.
Persons for Whom Routine HCV Testing Is of Uncertain Need
- Recipients of transplanted tissue (e.g., corneal, musculoskeletal, skin, ova, sperm)
- Intranasal cocaine and other non-injecting illegal drug users
- Persons with a history of tattooing or body piercing
- Persons with a history of multiple sex partners or sexually transmitted diseases
- Long-term steady sex partners of HCV-positive persons
Persons for Whom Routine HCV Testing Is Not Recommended
(unless they have risk factors for infection):
- Health-care, emergency medical, and public safety workers
- Pregnant women
- Household (nonsexual) contacts of HCV-positive persons
- General population