It is important to remember that the majority of patients with sexually transmitted diseases are asymptomatic.
Therefore, taking a sexual history can be very important. Please see my post How To Take A Sexual History – Help From The Centers For Disease Control And Prevention (CDC)
Posted on November 29, 2018 by Tom Wade MD.
The above post contains a script from the CDC that you can use to take your sexual history.
See also my post on When and How To Screen for Hepatitis B and C – Help From The CDC
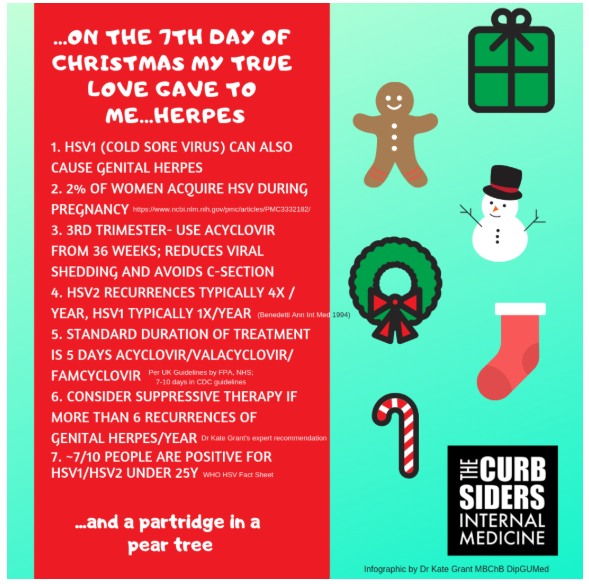
This post of excerpts from the Curbsiders” Episode #131 on herpes and from the CDC’s Genital Herpes – CDC Fact Sheet (Detailed). And I’ve added a reminder to myself that all sick newborns of less than 21 days should receive empiric iv acyclovir in addition to antibiotics for sepsis [from Approach To Febrile Infants In The Emergency Department lecture and accompanying slides from The Children’s Hospital of Philadelphia (CHOP)].
Here are the excerpts:
#133 Herpes for Everyone with Robert Bettiker MD
DECEMBER 24, 2018 By MATTHEW WATTO, MD
INCUBATION
Primary infection 2 days to 2 weeks (CDC STD Facts – Genital Herpes)
TRANSMISSION
After direct skin to skin contact with an infectious lesion on an infected individual. It cannot be caught from toilets,swimming pools, towels etc.
RECURRENT HERPES
After the primary infection, the virus becomes latent in a sensory nerve root ganglion and recurrent episodes occur when the HSV1/HSV2 virus reactivates. Usually the blisters recur in the site of the primary infection. Each time it reactivates, there is viral shedding, whether symptomatic or asymptomatic.
RECURRENCE RATES
HSV2 typically 4 times per year. HSV1 typically 1 time per year. (Benedetti Ann Int Med 1994; WHO HSV Fact Sheet)
Genital Herpes – CDC Fact Sheet (Detailed)
What is the link between genital herpes and HIV?
Genital ulcerative disease caused by herpes makes it easier to transmit and acquire HIV infection sexually. There is an estimated 2- to 4-fold increased risk of acquiring HIV, if individuals with genital herpes infection are genitally exposed to HIV. 13-15
How does genital herpes affect a pregnant woman and her baby?
Neonatal herpes is one of the most serious complications of genital herpes.5,16 Healthcare providers should ask all pregnant women if they have a history of genital herpes.11 Herpes infection can be passed from mother to child during pregnancy or childbirth, or babies may be infected shortly after birth, resulting in a potentially fatal neonatal herpes infection. 17 Infants born to women who acquire genital herpes close to the time of delivery and are shedding virus at delivery are at a much higher risk for developing neonatal herpes, compared with women who have recurrent genital herpes . 16,18-20 Thus, it is important that women avoid contracting herpes during pregnancy. Women should be counseled to abstain from intercourse during the third trimester with partners known to have or suspected of having genital herpes. 5,11
While women with genital herpes may be offered antiviral medication late in pregnancy through delivery to reduce the risk of a recurrent herpes outbreak, third trimester antiviral prophylaxis has not been shown to decrease the risk of herpes transmission to the neonate.11,21,22 Routine serologic HSV screening of pregnant women is not recommended. 11 However, at onset of labor, all women should undergo careful examination and questioning to evaluate for presence of prodromal symptoms or herpetic lesions. 11 If herpes symptoms are present a cesarean delivery is recommended to prevent HSV transmission to the infant.5,11,23 There are detailed guidelines for how to manage asymptomatic infants born to women with active genital herpes lesions.24
How is genital herpes diagnosed?
The preferred HSV tests for patients with active genital ulcers are detection of HSV DNA by nucleic acid amplification tests such as polymerase chain reaction (PCR), or isolation by viral culture.11 HSV culture requires collection of a sample from the lesion and, once viral growth is seen, specific cell staining to differentiate between HSV-1 and HSV-2.11,25,26 However, culture sensitivity is low, especially for recurrent lesions, and declines as lesions heal. 11,26 PCR is more sensitive, allows for more rapid and accurate results, and is increasingly being used. 25 Because viral shedding is intermittent, failure to detect HSV by culture or PCR does not indicate an absence of HSV infection. 11 Tzanck preparations are insensitive and nonspecific and should not be used. 11
For the symptomatic patient, testing with both virologic and serologic assays can determine whether it is a new infection or a newly-recognized old infection.26 A primary infection would be supported by a positive virologic test and a negative serologic test, while the diagnosis of recurrent disease would be supported by positive virologic and serologic test results.26
CDC does not recommend screening for HSV-1 or HSV-2 in the general population. 11 Several scenarios where type-specific serologic HSV tests may be useful include
- Patients with recurrent genital symptoms or atypical symptoms and negative HSV PCR or culture;
- Patients with a clinical diagnosis of genital herpes but no laboratory confirmation;
- Patients who report having a partner with genital herpes;
- Patients presenting for an STD evaluation (especially those with multiple sex partners);
- Persons with HIV infection; and
- MSM at increased risk for HIV acquisition.7
Please note that while type-specific herpes testing can determine if a person is infected with HSV-1 or HSV-2 (or both), there is no commercially available test to determine if a herpes infection in one individual was acquired from another specific person. CDC encourages patients to discuss any herpes questions and concerns with their health care provider or seek counsel at an STD clinic.
How can herpes be prevented?
Correct and consistent use of latex condoms can reduce, but not eliminate, the risk of transmitting or acquiring genital herpes because herpes virus shedding can occur in areas that are not covered by a condom.28,29
The surest way to avoid transmission of STDs, including genital herpes, is to abstain from sexual contact, or to be in a long-term mutually monogamous relationship with a partner who has been tested for STDs and is known to be uninfected.
Persons with herpes should abstain from sexual activity with partners when herpes lesions or other symptoms of herpes are present. It is important to know that even if a person does not have any symptoms, he or she can still infect sex partners. Sex partners of infected persons should be advised that they may become infected and they should use condoms to reduce the risk. Sex partners can seek testing to determine if they are infected with HSV.
Daily treatment with valacyclovir decreases the rate of HSV-2 transmission in discordant, heterosexual couples in which the source partner has a history of genital HSV-2 infection . 30 Such couples should be encouraged to consider suppressive antiviral therapy as part of a strategy to prevent transmission, in addition to consistent condom use and avoidance of sexual activity during recurrences.
Newborns in the first twenty-one days of life who are treated for suspected sepsis or other illnesses [eg seizures, etc] should be empirically treated with IV Acyclovir because:
- 75% of neonates with HSV are born to mothers without a history or clinical findings of HSV.
- 30% of neonates with HSV do not have skin vesicles – diagnosis delayed.
The above is from Approach To Febrile Infants In The Emergency Department lecture and accompanying slides from The Children’s Hospital of Philadelphia (CHOP).