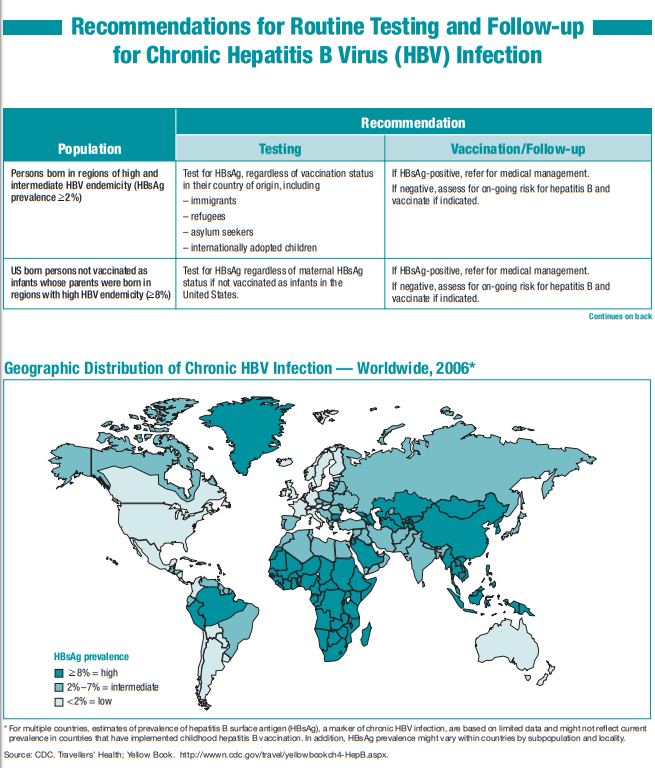
Here is the chart from the CDC, Recommendations for Routine Testing and Follow-up for Chronic Hepatitis B Virus (HBV) Infection [Link is to the printable PDF]:
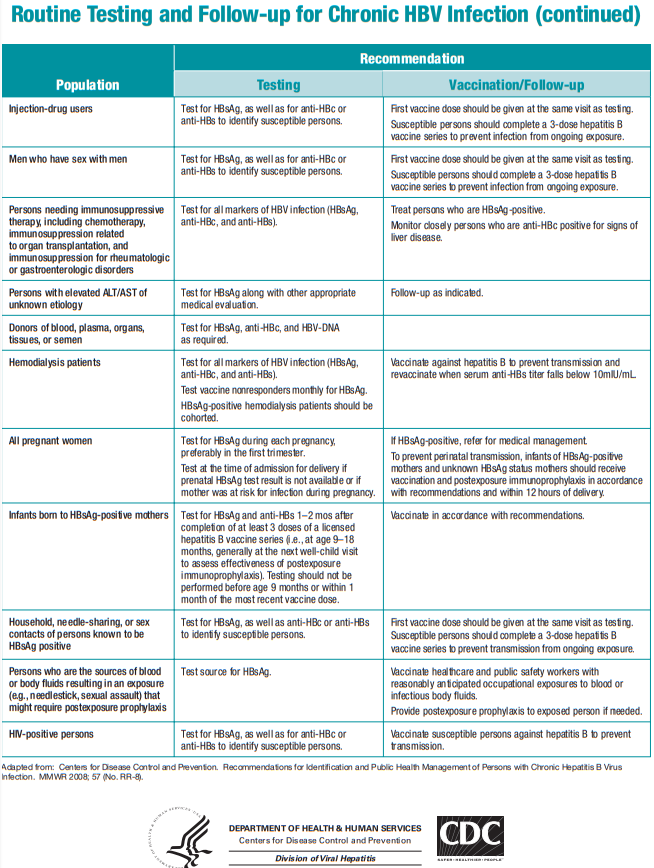
Here is the chart from the CDC, Interpretation of Hepatitis B Serologic Test Results [Link is to the printable PDF]:
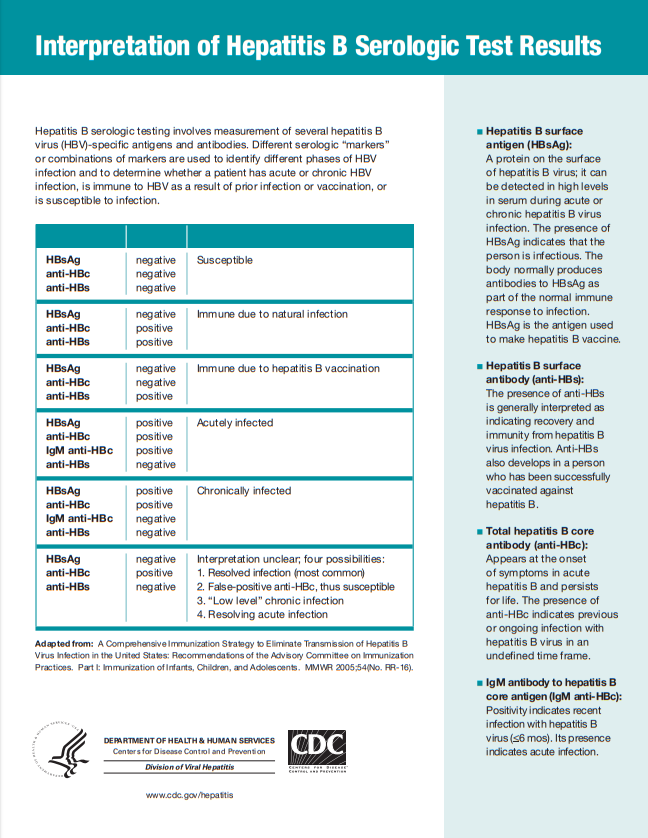
The above chart is great. And now onto the best resource on Hepatitis B I’ve ever encountered [Thanks, CoreIM!]:
This post contains the link to and excerpts from 5 Pearls on Chronic Hepatitis B, Part 1, Posted: January 17, 2018 from CoreIM
By: Dr. Amy Shen Tang, Dr. Martin Fried and Dr. Shreya P. Trivedi
Graphic: Dr. Mike Natter
Audio: Harit Shah
Here are the excerpts from the 5 Pearls podcast and show notes:
Quiz yourself on the following 5 Pearls on Chronic Hepatitis B (HBV)
Time Stamps
- 3:37 What are the most common ways HBV is transmitted and how can we use this to prioritize screening?
- Who is at risk for HBV reactivation?
- 10:48 What tests do you order when screening for HBV?
- In which populations is HBV vaccination recommended?
- 13:55 What are the four possible meanings of an isolated positive total anti-HBc?
- 15:01 In an asymptomatic adult, is it necessary to send an anti-HBc IgM to distinguish acute from chronic HBV infection?
- 16:19 What are the implications of seroconversion of HBeAg from positive to negative?
Show Notes
Pearl 1:
- HBV screening is based on transmission and reactivation risks.
- You can think about three high risk screening groups based on modes of HBV transmission:
- Mother to child: All people born in regions with > 2% HBV prevalence. This includes the entire continents of Asia and Africa, parts of South America, the Middle East, and Eastern Europe. Plus all pregnant women.
- Sexual transmission: Household contacts & sexual partners of people with HBV, men who have sex with men
- Needle-sharing: Current and former IV drug users, hemodialysis patients
- Before starting a biologic agent, chemotherapy or hepatitis C treatment, screen for HBV; these agents may predispose to HBV reactivation.
- HBV reactivation can cause liver failure and even death.
- Screen for HBV when starting treatment for HIV and HIV preexposure prophylaxis (PREP) as there are medications (such as tenofovir) used for both HIV and HBV.
- Fun Fact: HBV can live outside of the body in dried blood for at least 7 days!
- Counsel chronic HBV infected patients about NOT sharing toothbrushes or razors. All blood spills should be cleaned with bleach.
Pearl 2:
- Screen for HBV with HBV surface antigen (HBsAg), surface antibody (anti-HBs) and total core antibody (anti-HBc)
- If a patient is HBsAg negative and anti-HBs positive, a total core antibody will indicate if the patient is immune from prior vaccination or prior infection and living with the virus dormant in their liver, making them at a risk for reactivation
- Vaccinate all populations at high-risk (see Pearl 1), all diabetics, sexually active people NOT in a long-term, monogamous relationship, health care personnel, international travelers to regions with intermediate or high HBV prevalence and all other people who wish to be protected from HBV infection.
Pearl 3:
- Four meanings of a positive total anti-HBc with a negative anti-HBs and HBsAg:
- The majority of patients with an isolated total anti-HBc have been infected in the past and just have undetectable levels of anti-HBs
- You may consider measuring HBV DNA to see if the patient has occult infection, which is less common (~8%).
- It may also mean the patient is in the “window phase” with a resolving an acute infection and anti-HBs hasn’t formed yet.
- A false-positive anti-HBc is also possible but rare with modern assays.
Pearl 4:
- In asymptomatic patients from endemic areas screened for HBV, a positive HBsAg implies chronic infection. IgM anti-HBc is not required to confirm chronic infection.
- Immunocompetent adults acutely infected with HBV are more likely to show symptoms and less likely to develop chronic infection, whereas young children or immunosuppressed persons are less likely to have symptoms of acute infection and more likely to develop chronic infection.
Pearl 5:
- HBeAg is a marker of active replication and increases risk of viral transmission and hepatocellular carcinoma.
- The majority of people infected with HBV perinatally will seroconvert from HBeAg positive to negative around 30 years of age. HBeAg seroconversion is associated with decrease in viral load levels and lower rates of hepatocellular carcinoma (HCC)
- A subset of HBeAg negative patients can develop mutations in the HBV genome that is integrated into the patient’s hepatocytes, leading to increasing viral replication and risk for HHC.
The References at the end of CoreIM’s post, 5 Pearls on Chronic Hepatitis B, Part 1, cover all the aspects of Hepatitis B Screening and Prevention in great depth.
For a great podcast and post on chronic Hepatitis B management, see 5 Pearls on Chronic Hepatitis B, Part 2 Management
Posted: January 31, 2018
By: Dr. Amy Shen Tang, Dr. Martin Fried and Dr. Shreya P. Trivedi
Graphic: Dr. Amy Ou, Dr. Michelle Lo
Audio: Harit Shah