First watch the YouTube video, Autoimmune Encephalitis – an Overview, Feb 20, 2020 from The Encephalitis Society:
And here are links to and excerpts from SOP: antibody-associated autoimmune encephalitis [PubMed Abstract] [Full Text HTML] [Download Full Text PDF]. November 2020 Neurological Research and Practice 2(1)
And here are excerpts:
Abstract
Background: Antibody-mediated and paraneoplastic autoimmune encephalitides (AE) present with a broad
spectrum of clinical symptoms. They often lead to progressing inflammatory changes of the central nervous system
with subacute onset and can cause persistent brain damage. Thus, to promptly start the appropriate and AEspecific therapy, recognition of symptoms, initiation of relevant antibody diagnostics and confirmation of the
clinical diagnosis are crucial, in particular as the diseases are relatively rare.Aim: This standard operating procedure (SOP) should draw attention to the clinical presentation of AE, support the
diagnostic approach to patients with suspected AE and guide through the necessary steps including therapeutic
decisions, tumour screening and exclusion of differential diagnoses.Method: Based on existing diagnostic algorithms, treatment recommendations and personal experiences, this SOP
gives an overview of clinical presentation, diagnostic procedures and therapy in AE. Additional information is
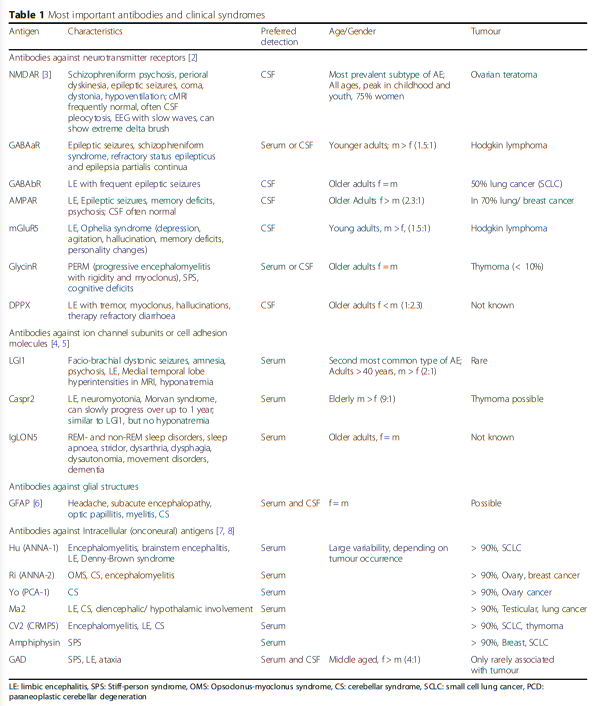
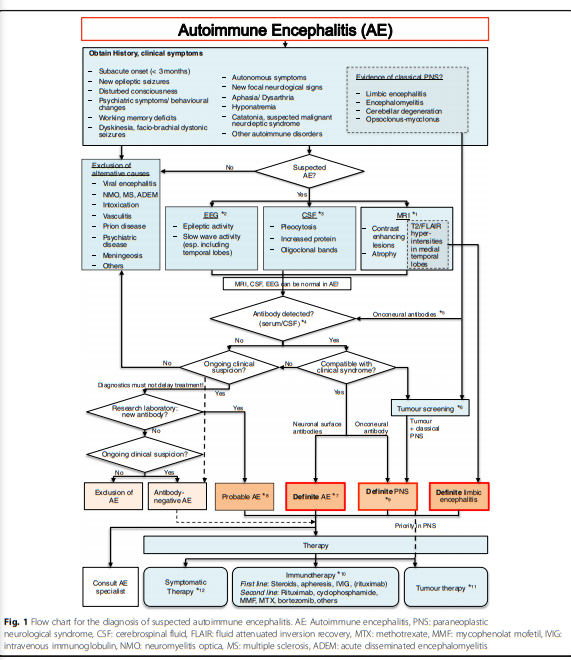
provided within an accompanying text and a table describing the most important autoantibodies and their characteristics.Results: The initial steps of the AE flow chart are based on clinical symptoms and the patient’s history. Assignment
to paraneoplastic or antibody-mediated AE is sometimes clinically possible. Diagnostics should include MRI, EEG
and CSF analysis with antibody panel diagnostic. Definite AE can be diagnosed if the underlying antibody is
compatible with the clinical presentation. Classification of probable AE may be possible even with negative antineuronal autoantibodies if the clinical presentation and laboratory abnormalities are highly suggestive of AE. The
confirmed AE diagnosis requires immediate initiation of immunotherapy.Conclusion: The SOP facilitates the recognition of patients with AE and presents the necessary diagnostic and
therapeutic steps.Keywords: Autoimmune, Encephalitis, Limbic encephalitis, Antibody, Paraneoplastic, NMDAR
The figure below is from the article:
The figure below is from the article:
Here is the link to Autoimmune Encephalitis: What Psychiatrists Need to Know
January 29, 2020
Pojen Deng, MD , Anusha Yeshokumar, MD from Psychiatric Times.
Here are excerpts:
The figure below is from the article:
The figure below is from the article:
Clinical assessment of autoimmune encephalitis
Mental health professionals evaluating a case of new onset psychosis should be aware of the expert-consensus suggested diagnostic criteria for autoimmune encephalitis.7
Diagnosis can be made when all three of the following criteria have been met:
1 Subacute onset (rapid progression of less than 3 months) of working memory deficits (short-term memory loss), altered mental status (lethargy, personality change, or cognitive deficits), or psychiatric symptoms
2 At least one of the following: new focal CNS findings; seizures not explained by a previously known seizure disorder; cerebrospinal fluid (CSF) pleocytosis (white blood cell count of more than five cells per mm); MRI features suggestive of encephalitis.
3 Reasonable exclusion of alternative causes
Psychiatric practitioners should also take note of any of the following features in psychiatric illness, which would prompt concern for encephalitis:
• Focal neurologic deficits, including hyper-reflexia or signs of meningismus
• Concurrent dysautonomia (ie, tachycardia, hypertension, hypotension, fevers)
• Prominent symptoms such as headache or flu-like illness
• New onset catatonia without prior psychiatric history or rapid progression to catatonia
• Refractory psychosis or catatonia to appropriate psychotropic management
• Cognitive deficits that appear out of proportion to duration of psychiatric illness or out of proportion to general psychiatric symptoms
• New onset psychosis developing rapidly without family history, not substance related, and without prodromal symptoms
Clinicians should note that these recommendations are most pertinent for cases of new onset psychosis, and unusual symptoms to be evaluated for most closely overlap with the presenting features of anti-NMDA receptor encephalitis.
As detailed above, the primary flags are the presence of seizures, dyskinesias, and dysautonomia concurrent with mood symptoms or psychotic features. Other cases that may be considered may have early manifestation of or rapid progression to unusual psychiatric features in a primary psychotic illness, such severe agitation and catatonia, or psychosis and catatonia refractory to appropriate psychotropic management.