In addition to the resource in this post below, please see ESC Council on hypertension position document on the management of hypertensive emergencies [PubMed Abstract] [Full Text HTML] [Full Text PDF]. Eur Heart J Cardiovasc Pharmacother. 2019 Jan 1;5(1):37-46.
I’ve divided these my study notes on the European high blood pressure guidelines into several parts for ease of my review. Links to all my post on the 2018 European Hypertension Guidelines are in Additional Resources after this post.
The following are Hypertension Urgencies And Emergencies section from the 2018 ESC/ESH Guidelines for the management of arterial hypertension [PubMed Abstract] [Full Text HTML] [Full Text PDF]. Eur Heart J. 2018 Sep 1;39(33):3021-3104. doi: 10.1093/eurheartj/ehy339:
8.3 Hypertension urgencies and emergencies
Hypertension emergencies are situations in which severe hypertension (grade 3) is associated with acute HMOD, which is often lifethreatening and requires immediate but careful intervention to lower BP, usually with intravenous (i.v.) therapy.398 The rate and magnitude of an increase in BP may be at least as important as the absolute level of BP in determining the magnitude of organ injury.399 Typical presentations of a hypertension emergency are:
• Patients with malignant hypertension, characterized by
severe hypertension (usually grade 3) associated with funduscopic changes (flame haemorrhages and/or papilloedema), microangiopathy, and disseminated intravascular coagulation, and can be associated with encephalopathy (in about 15% of cases),400 acute heart failure, and acute deterioration in renal function. The hallmark of this condition is small artery fibrinoid necrosis in the kidney, retina, and brain. The term ‘malignant’ reflects the very poor prognosis for this condition if untreated.401–404
• Patients with severe hypertension associated with other
clinical conditions who are likely to require an urgent reduction of BP, e.g. acute aortic dissection, acute myocardial ischaemia, or acute heart failure.
• Patients with sudden severe hypertension due to phaeochromocytoma, associated with organ damage.
• Pregnant women with severe hypertension or preeclampsia (see section 8.9.1).The most common emergency symptoms will depend of the
organs affected but may include headache, visual disturbances, chestpain, dyspnoea, dizziness, and other neurological deficits. In patients with hypertensive encephalopathy, the presence of somnolence, lethargy, tonic clonic seizures, and cortical blindness may precede a loss of consciousness; however, focal neurological lesions are rare and should raise the suspicion of stroke.Acute stroke, especially intracerebral haemorrhage, when
associated with severe hypertension has often been termed a hypertension emergency, but a more cautious approach is now recommended for acute BP lowering in the emergency setting of acute stroke (see section 8.15).The term ‘hypertension urgency’ has also been used to describe
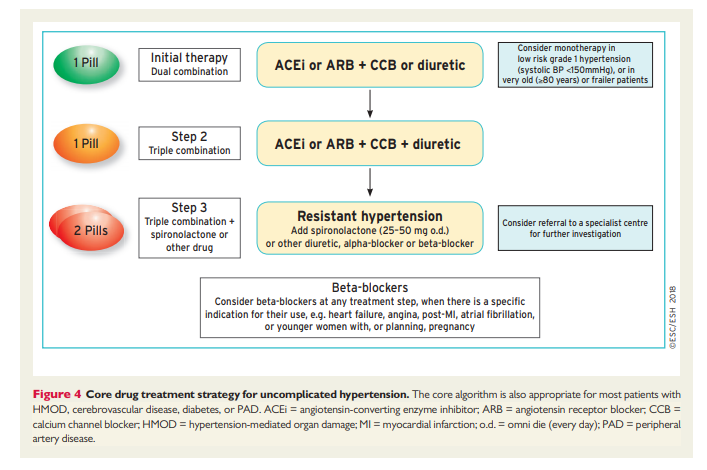
severe hypertension in patients presenting to the emergency department in whom there is no clinical evidence of acute HMOD.405 Whilst these patients require BP reduction, they do not usually require admission to hospital, and BP reduction is best achieved with oral medication according to the drug treatment algorithm presented in Figure 4. However, these patients will require urgent outpatient review to ensure that their BP is coming under control.
Acute and severe increases in BP can sometimes be precipitated
by ingestion of sympathomimetics such as meta-amphetamine or cocaine. This can result in a hypertension emergency when there is evidence of acute HMOD.It is emphasized that many patients in an emergency department with acute pain or distress may experience an acute elevation in BP that will be restored to normal when the pain and distress are relieved, rather than requiring any specific intervention to lower BP.
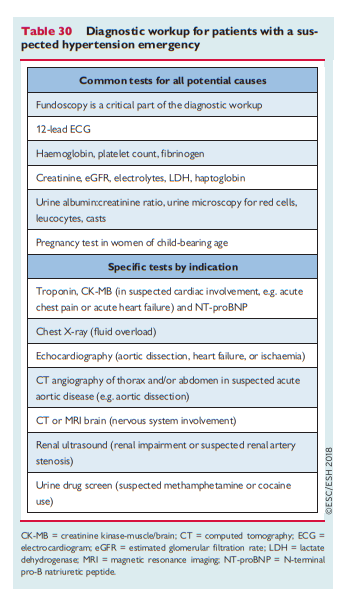
For patients with a suspected hypertension emergency, a diagnostic workup is shown in Table 30.
8.3.1 Acute management of hypertensive emergencies
Apart from acute BP lowering in stroke, there are no RCTs evaluating different treatment strategies for hypertensive emergencies. The key considerations in defining the treatment strategy are:
(1) Establishing the target organs that are affected, whether they require any specific interventions other than BP lowering, and whether there is a precipitating cause for the acute rise in BP that might affect the treatment plan (e.g. pregnancy);
(2) The recommended timescale and magnitude of BP lowering
required for safe BP reduction;(3) The type of BP-lowering treatment required. With regard to drug treatment, in a hypertension emergency, i.v. treatment with a drug with a short half-life is ideal to allow careful titration of the BP response to treatment in a higher dependency clinical area with facilities for continuous haemodynamic monitoring.
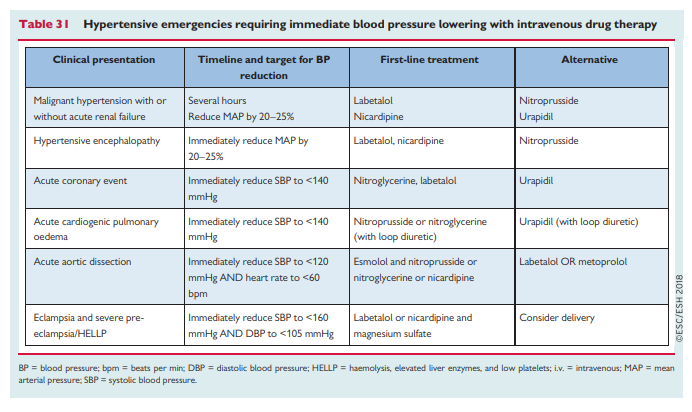
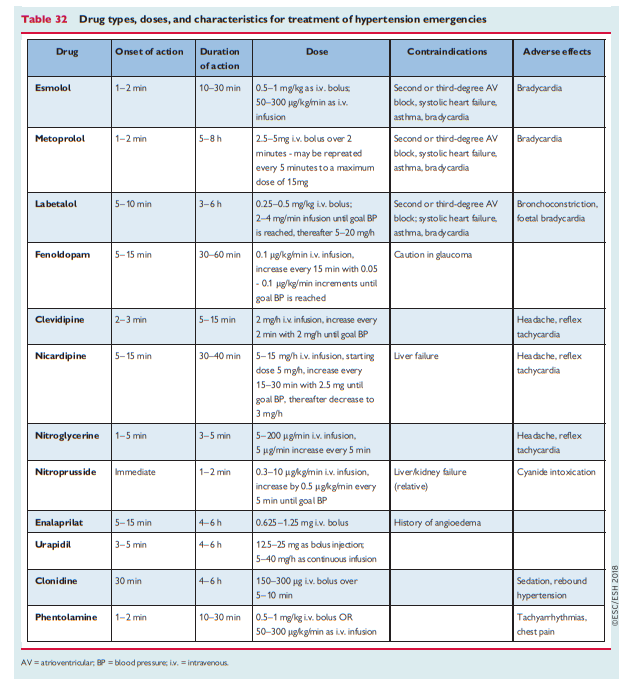
Recommended drug treatments for specific hypertension emergencies 398,406 are shown in Table 31 and an expanded range of possible drug choices 398 is shown in Table 32. Rapid uncontrolled BP lowering is not recommended as this can lead to complications.397
8.3.2 Prognosis and follow-up
The survival of patients with hypertension emergencies has improved dramatically over past decades,407 but these patients remain at high risk408,409 and should be screened for secondary hypertension (see section 8.2). After discharge from hospital, when BP has reached a safe and stable level on oral therapy, we recommend frequent, at least monthly, visits in a specialized setting until the optimal target BP is achieved and long-term specialist follow-up thereafter.