See also my blog post, Head and Neck Injury Imaging Guidelines from NICE For Adults and Children posted on May 18, 2014. The head injury imaging guideline is from the National Institute for Health and Care Excellence, 2014. ‘Head injury’, NICE clinical guideline 176. London: National Clinical Guideline Centre.
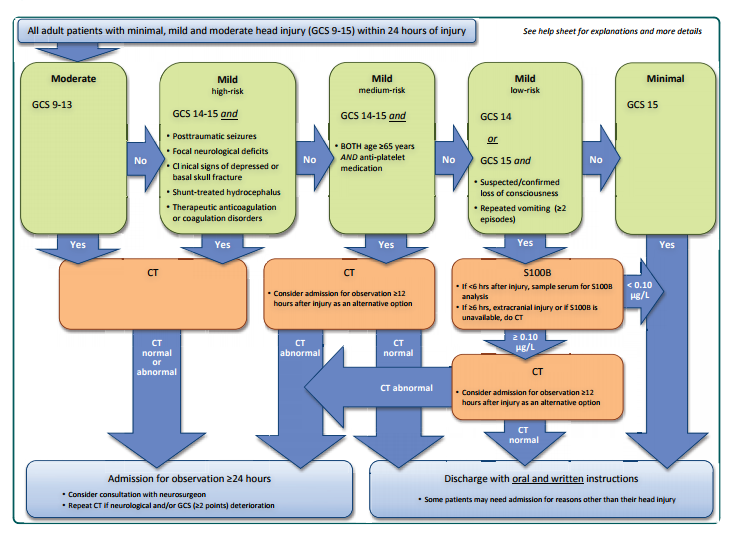
The following figure is from The Scandinavian guidelines for initial management of minimal, mild and moderate head injuries in adults:an evidence and consensus-based update [BioMed Central Full Text HTML] [BioMed Central Full Text PDF] 2013.
[See also the commentary on the above guideline, New guidelines for the initial management of head injury [Biomed Central Full Text HTML] [Biomed Central Full Text PDF] 2013]
What follows are some excerpts from the Scandinavian Guidelines:
Clinical question 1: ‘Which adult patients with minimal, mild and moderate head injury need a head CT and which patients may be directly discharged?’
(1) We recommend that adult patients after mild and moderate head injury with GCS ≤14, loss of consciousness, repeated (≥2) vomiting, anticoagulant therapy or coagulation disorders, clinical signs of depressed or basal skull fracture, post-traumatic seizures or focal neurological deficits should have a CT scan (moderate quality, strong recommendation).
(2) We recommend that adult patients after mild head injury with GCS 14 and no risk factors (anticoagulant therapy or coagulation disorders, post-traumatic seizures, clinical signs of depressed or basal skull fracture, focal neurological deficits), or GCS 15 with loss of consciousness or repeated (≥2) vomiting and no other risk factors, be sampled for analysis of S100B if less than 6 h have elapsed following trauma. If S100B is less than 0.10 μg/l, the patient may be discharged without a CT (moderate quality, strong recommendation).
(3) We recommend that adult patients after minimal and mild head injury with GCS 15 and without risk factors (loss of consciousness, repeated (≥2) vomiting, anticoagulation therapy or coagulation disorders, posttraumatic seizures, clinical signs of depressed or basal skull fracture, focal neurological deficits) can be discharged from the hospital without a CT scan (moderate quality, strong recommendation)
Clinical question 2: ‘Which adult patients with minimal, mild and moderate head injury need in-hospital observation and/or a repeat head CT?’
(1) We suggest that all adult patients after head injury
with GCS ≤13, clinical signs of depressed or basal skull
fracture, anticoagulation therapy or coagulation disorder,
post-traumatic seizure or focal neurological deficit
should have a CT scan and be admitted to hospital for
observation, irrespective of CT findings (low quality,
weak recommendation).(2) We recommend that repeat CT scans should be performed
in patients with neurological and/or GCS (≥2 points) deterioration (low quality, strong recommendation).For the first time, a brain biomarker has been introduced into clinical practice guidelines. Using a low cutoff of 0.10 μg/l, the biomarker has shown considerable ability to predict the absence of CT pathology and neurosurgical intervention [36,41,42]. This negative prediction is welcomed since all other risk factors are of positive predictive nature. S100B allows for a safe reduction in CT scans in a subpopulation of patients with mild head injury. In order to maintain the theoretical safety and cost-saving ability, the biomarker should primarily not exhibit false negative results. Also, the biomarker should only be taken in patients that would usually receive a CT scan and the fraction of negative S100B results (below cut-off) should be as large as possible. S100B is clinically unspecific [43,44] and has a short half-life [45]. Therefore, patients with extracranial injuries and those seeking care more than 6 h after trauma are not good candidates for S100B sampling due to a risk of false positives and negatives, respectively. Some patients have risk factors with higher predictive abilities and also factors that would usually warrant admission irrespective of CT findings. This group is therefore also not suitable for S100B sampling. Despite the relatively good evidence for S100B in this setting, biomarkers have historically had different effects in actual management and the clinical impact and health economic implications may alter future recommendations. Based upon the current evidence and clinical setting, however, this biomarker should safely reduce resource use if used correctly since low levels are very uncommon in patients needing neurosurgical intervention in this setting.