In addition to today’s outstanding resource, please see and review:
- Gold Global Initiative for Chronic Obstructive Lung Disease 2023
- GLOBAL STRATEGY FOR THE DIAGNOSIS, MANAGEMENT,
AND PREVENTION OF CHRONIC OBSTRUCTIVE PULMONARY
DISEASE (2023 REPORT) - 2023 EXECUTIVE SUMMARIES
- GLOBAL STRATEGY FOR THE DIAGNOSIS, MANAGEMENT,
- COPD Educational Video Series
- Our videos are designed to provide education and awareness for people affected by Chronic Obstructive Pulmonary Disease (COPD). These include patients, their families, and caregivers. The videos also serve as an exceptional resource for healthcare professionals to convey education.
- Inhaler Education
“These are videos of inhalers approved for the treatment of COPD depicting their proper use.” - Nebulizer Education
“These are videos that will show you how to use, clean and store the most common types of nebulizers.”
- Inhaler Education
- Our videos are designed to provide education and awareness for people affected by Chronic Obstructive Pulmonary Disease (COPD). These include patients, their families, and caregivers. The videos also serve as an exceptional resource for healthcare professionals to convey education.
- Alpha-1 Foundation
- What is Alpha-1?
- “Alpha-1 Antitrypsin Deficiency (Alpha-1) is a genetic condition that can cause damage to the lungs and/or the liver. There is no cure for Alpha-1, but some symptoms can be managed with treatment.”
- Testing & Diagnosis
- “Alpha-1 Antitrypsin Deficiency (Alpha-1) can be diagnosed with a simple blood test.”
- “Who should be tested for Alpha-1? The latest clinical guidelines recommend Alpha-1 testing for:
- People with COPD (chronic obstructive pulmonary disease), a group of lung diseases, including emphysema, that block airflow and make it difficult to breathe
- People with unexplained chronic liver disease
- People with panniculitis, a skin condition that some people with Alpha-1 develop
- Parents, siblings, children, and extended family members of people diagnosed with Alpha-1″
- What is Alpha-1?
- About COPD and Bronchiectasis (COPD-Bronchiectasis Overlap)
- “Although COPD and bronchiectasis are related diseases and airway clearance techniques are helpful for both conditions, the medications and other treatments used for COPD and bronchiectasis are different.”
- “It is very important if you have cough that produces a lot of phlegm (also known as mucus or sputum) and experience repeated lung infections, that you ask your health care provider to test you for bronchiectasis (usually diagnosed with a CT scan), COPD or both”.
Today, I reviewed and link to, embed, and excerpt from The Curbsiders‘ #408 COPD in Older Adults with Leah Witt, MD & Amber Lanae Martirosov, PharmD.
Definitions, 4Ms & Inhaler Pro Tips Level up COPD management in older adults. Start with learning the latest in COPD diagnosis and classification, then stay for the mind-blowing inhaler misuse & cost discussion. We’re joined by a dynamic (and interprofessional) duo: Dr. Leah Witt (@leahjwitt) and Dr. Amber Lanae Martirosov, PharmD (@AmberMartirosov).
All that follows is from the excellent show notes.
Show Segments
- Intro
- Rapid Fire Questions
- Case Part 1
- COPD Definition
- COPD alphabet soup: ABE
- Case Part 2
- Geriatric 4Ms & COPD
- Inhaler Use & Cost
- Outro
COPD in Older Adults Pearls
- The diagnosis of COPD is a clinical one– you must have the appropriate history, exposure and spirometry to make the diagnosis!
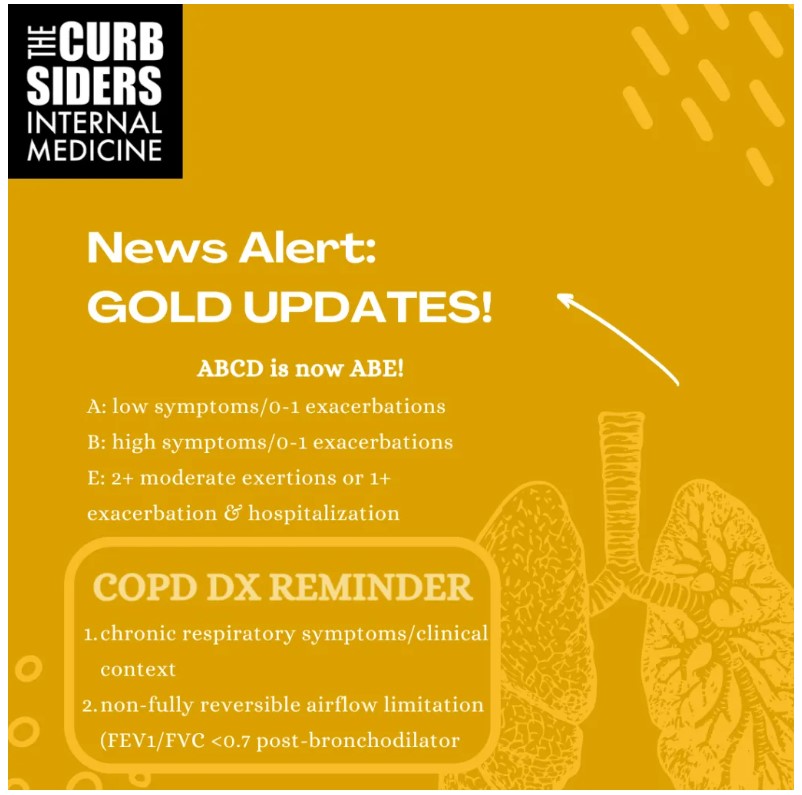
- Update your COPD alphabet: ABCD is now ABE with a focus on exacerbations.
- The natural history of lung aging includes thoracic cage changes, reduced elastic recoil, and reduced respiratory muscle strength
- Learn the Age-Friendly 4Ms to up-level your care of chronic lung disease (and any chronic disease for that matter).
- Supplemental oxygen use may increase the risk for social isolation and loneliness, and has no demonstrated mortality benefit for those with moderate hypoxemia (desaturation only with exertion).
- The cost of inhalers, incorrect inhaler use, side effects of treatment and polypharmacy all affect drug adherence and disease control.
COPD in Older Adults
COPD Definitions & Classification
What is COPD?
Chronic obstructive pulmonary disease (COPD): a heterogeneous condition characterized by:
- CHRONIC respiratory symptoms (shortness of breath, cough, sputum production)
due to airway and/or alveolar abnormalities (eg chronic bronchitis, bronchiolitis and emphysema) with the appropriate clinical context (eg exposure such as tobacco use/exposure or air pollution)
- persistent, sometimes progressive airflow obstruction (as diagnosed by airflow limitation (FEV1/FVC <0.7 post bronchodilation). (GOLD Report 2023)
Think it’s COPD? Get spirometry and imaging (at least a chest x-ray), though depending on your differential diagnosis additional work-up may be appropriate (asthma, bronchiectasis, ILD, and CHF are just some of the diseases typically on the differential diagnosis list). Asthma and COPD can be difficult to distinguish in the older adult. Asthma alone typically has reversible airflow obstruction with bronchodilators though this may become less reversible with age. Other signs of asthma are a history of childhood asthma, atopic symptoms and/or elevated eosinophils or IgE (type 2 inflammation). Asthma and COPD can overlap (Postma 2015).
ABE (COPD alphabet soup)
In 2011, GOLD recommended assessing COPD by more than just obstruction severity on spirometry, but also grading by symptom level, e.g. based on modified Medical Research Council dyspnea scale (mMRC) or COPD Assessment Test (CAT) and exacerbation history. This assessment tool was called ABCD (A and B being low exacerbation groups and low or high symptoms respectively, C and D being high exacerbation groups with low or high symptoms). In 2023, groups C and D were merged into a single group called “E” to highlight the importance of exacerbations to guide treatment decisions! (GOLD Report 2023)
Natural History of Lung Aging
Maximal lung function is achieved in the third decade of life. Prenatal and early childhood exposures such as parental smoking, air pollution and respiratory infections all affect achievement of maximal lung function (Janssens 1999, Janssens 2005, Ito 2009, Bode 1976).
Possible age-related changes in the pulmonary system individually vary and can include
- Chest wall compliance changes: eg kyphosis related to osteoporosis/vertebral compression fractures, rib cage/cartilage calcification
- Parenchymal distortion and reduced elastic recoil
- Weakening respiratory muscles (sarcopenia) including the principal muscles of respiration (diaphragm and external intercostals) and accessory muscles (sternocleidomastoid, scalenes). The maximum inspiratory pressure and maximum expiratory pressure decline with age. (These pressure values can be measured in a pulmonary function laboratory).
How does age affect COPD diagnosis?
There is a risk of overdiagnosis of COPD in older adults, since spirometry may look more obstructive with age (Janssens 2005, GOLD Report 2023)
How this impacts spirometry on average is that spirometry is usually more obstructive. The GOLD guidelines address this and acknowledge that using a lower limit of normal cut off would be better for older adults (and younger adults who might be under-diagnosed), but they’re committed to sticking to the FEV1/FVC <0.7 post-bronchodilator, because it is simple and independent of reference values. The problem with using lower limit of normal (LLN) of references values is that they depend on the choice of reference equations and we don’t have great data validating the use of LLN.
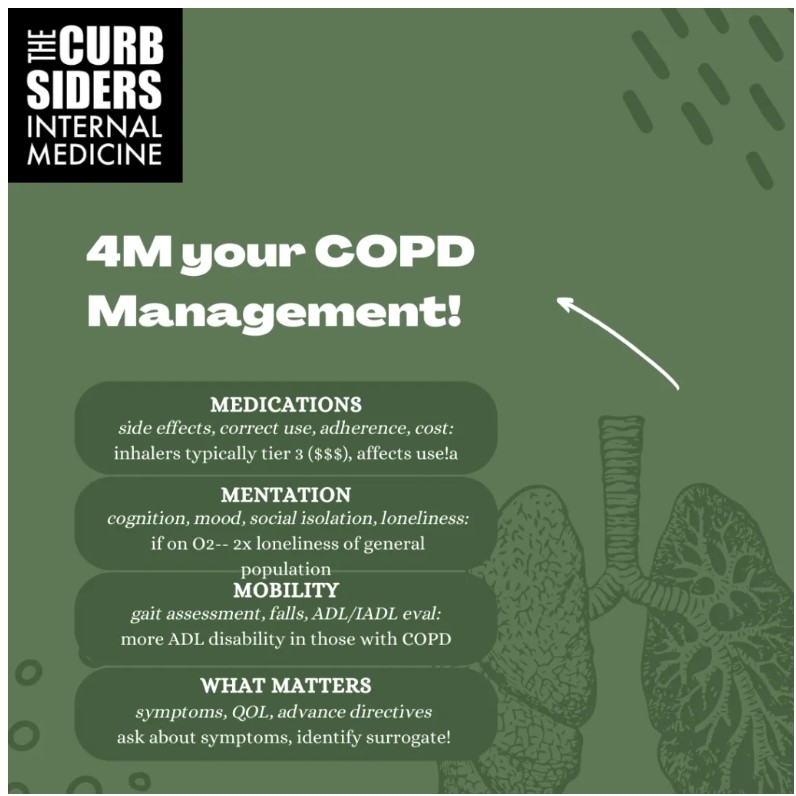
4Ms & Age-Friendly Chronic Lung Disease Management
The 4Ms Framework for Age-Friendly care, developed by the John A Hartford Foundation and Institute for Healthcare Improvement, is a great framework for geriatricizing your care of older adults with chronic disease.
Medications
This covers appropriate prescribing, correct use of the inhaler device, regularly reviewing and addressing of the side effects, discussing costs and strategies for cost containment of the treatments. The updated 2023 GOLD Report reads much more like an age-friendly manual– they’ve added sections on issues related to inhaled delivery including adherence and choice of device! (GOLD Report 2023)
Older adults are at risk for polypharmacy (more medications and medication administration types). This has been demonstrated in COPD. Older adults with COPD have more moderate polypharmacy (4+ meds, 80.6 vs 58.4%, OR 2.7, 2.0-3.8) and severe polypharmacy (10+ meds, 37.5% vs 16.1% OR 2.9, 2.0-4.2) (Witt 2022).
Mentation
Mentation includes considering cognitive impairment/dementia, mood disorders, delirium, and social isolation/loneliness. National prevalence of social isolation and loneliness is high among those with COPD– a recent study showed nearly 1 in 6 adults with COPD experience social isolation, and 1 in 5 experience loneliness, with almost twice the prevalence among those on supplemental oxygen compared to the general population (Suen 2023).
Cognitive impairment is also more common in COPD. In previous studies, people who were hypoxemic were more likely to have cognitive impairment and regular use of oxygen decreases risk for cognitive impairment (Thakur 2010, Dodd 2010).
Mobility
The Mobility “M” includes gait and falls assessment, frailty evaluation and ADL/IADL impairments. Community-dwelling adults with COPD have high rates of ADL disability, even after adjusting for comorbidities and age (OR 2.5 of at least one ADL deficit, 95% CI 1.9, 3.4, p<0.0001) (Witt 2022).
Pulmonary rehab is very important (and one of Paul’s favorite board question answers)—at all ages people benefit from pulmonary rehab including those over age 80! In Medicare beneficiaries hospitalized for a COPD exacerbation, those who started pulmonary rehab within 90 days of discharge had lower risk of death in the following year (and there was a dose effect meaning more pulmonary rehab means lower risk of death!) (Lindenauer 2020, Jain 2023).
Oxygen tubing is a fall risk. Prescribing oxygen should involve a risk/benefit discussion– continuous supplemental oxygen confers a mortality benefit for people with severe resting desaturation (defined as PaO2 ≤55 (SaO2≤88%) or PaO2 ≤59 (SaO2≤89%) with RV failure or Hct≥55 (NOTT 1980). However, there are significant uncertainties about the benefit of supplemental O2 with moderate resting hypoxemia, exercise-related hypoxemia and nocturnal hypoxemia. A 2016 study looked at patients with moderate resting hypoxemia and exercise-related hypoxemia (though excluded people who desaturated <80%) and there was no mortality or hospitalization benefit (nor quality of life benefit) (LOTT 2016). Other studies have suggested a potential palliative, exercise and cognitive benefit (Davidson 1988, Tarpy 1995). TL;DR: the jury is still out regarding the benefit (or lack thereof) conferred by supplemental oxygen for many of the common indications it is often prescribed.What Matters
This M focuses on understanding and aligning care with each older adult’s specific care preferences. We talked about this in episode 295 with Rebecca Sudore– Identifying a surrogate decision-maker and talking about expectant management is key, such as planning for future hospitalizations due to exacerbations. As is exploring overall goals and preferences for care as part of routine management.
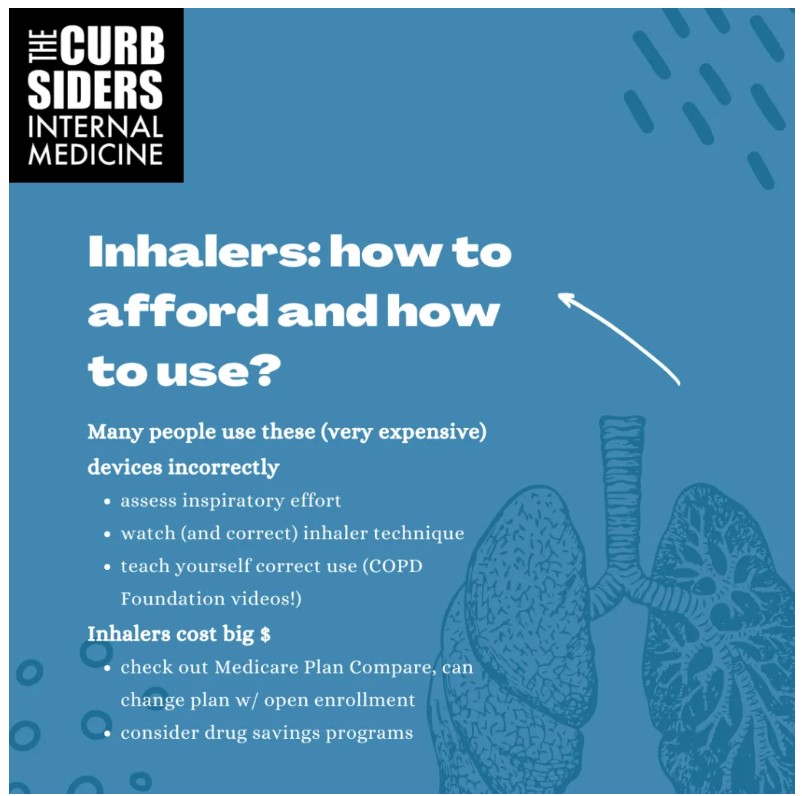
Inhalers: Expensive and Incorrectly used
Inhaler Choice
If you’re starting from scratch, consider prescribing by GOLD group. Group A (low symptoms/few exacerbations) can start with “a bronchodilator”– your choice! Starting with a LAMA (long-acting muscarinic agent) is a good choice because it can also help “dry up secretions” (expert opinion, Dr. Martirosov). If in Group B (high symptoms, few exacerbations), consider starting with a long acting beta agonist (LABA)/LAMA combination, which is the same guidance for Group E (high exacerbations). An inhaled corticosteroid can be added if blood eosinophils are elevated (≥300) (or of course if there is asthma/COPD overlap). In our patient’s case, she was actually in Group E but was sent home with tiotropium alone (a LAMA). Since she has the medication already, and isn’t using it correctly, focus on perfecting technique before doing more inhaler switcharoos–you can always step up/down therapy with time. It’s also a tough sell to get people to discard a newly purchased and expensive inhaler, just because the prescribing wasn’t perfectly guideline driven on the first try! (expert opinion, Dr. Witt)
Inhaler Use
Optimal COPD management is significantly affected by incorrect inhaler use and adherence issues to polypharmacy, cost of medications, and side effects.
It is CRITICAL that providers understand how to use inhalers themselves (to be better teachers!) and learn the basics of the cost of inhalers. Inhalers are frequently used incorrectly (Sanchis 2016). Watch inhaler videos on YouTube from the COPD Foundation and download their app for treatment algorithms based on disease severity, as well as a list of inhaler options. Print out some inhaler posters for your clinic to help patients identify their devices (American Lung Association, Asthma & Allergy Network). Watch patients use their inhaler, and correct their technique.
Further, inadequate inspiratory flow can affect inhaler efficacy. Amber suggests two devices to assess this: 1. Vitalograph or 2. In-Check Dial (Blum 2018). Cognitive impairment can be a barrier to learning correct use, and in these cases, nebulized treatments may be more effective.
Costs
High medication costs are a difficult and complicated challenge, and lead to reduced adherence. Annual out of pocket costs for inhalers while on average part D plans have been projected to be at least $900/year for one inhaler (Tseng 2017). People who pay >$20/month for an inhaler are at high risk for cost-related non-adherence (Castaldi 2010).
It is important to query patients about the cost of medications as this affects adherence. Learn more about prescription drug coverage, particularly the Medicare Part D program. There are many Medicare Part D plans and plans can be changed during the annual open enrollment period in the fall. Patients may use the Medicare Plan Compare website to help them compare different plans. Physicians can work with pharmacies to identify lower cost alternatives. Some drug manufacturers also have patient assistance programs for patients whose income is below their set threshold. And advocacy to reduce drug costs is imperative (Patel 2018)– did you know that device patents are responsible for manufacturers maintaining market exclusivity on brand-name inhalers (Demkowicz 2023)?