Today, I review and excerpt from the Ejection Section of
- The “5Es” of emergency physician-performed focused cardiac ultrasound: a protocol for rapid identification of effusion, ejection, equality, exit, and entrance [PubMed Abstract] [Full-Text HTML] [Full-Text PDF]. Acad Emerg Med. 2015 May;22(5):583-93. doi: 10.1111/acem.12652. Epub 2015 Apr 22.
All that follows is from the above resource.
Ejection
The second “E” in our protocol is assessment of LV ejection fraction (LVEF). This E can help differentiate causes of hypotension, chest pain, and dyspnea and may aid in expediting condition-specific therapies.3, 25, 26
There are multiple quantitative modalities for LVEF calculation; however, qualitative estimates of ejection fraction by EP FOCUS correlate well with both quantitative measurements and subjective estimates by cardiologists.25, 27 Qualitative assessment of global ejection is typically categorized as “hyperdynamic” (LVEF > 65%), “normal” (LVEF 50% to 65%), “moderately depressed” (LVEF 30% to 50%), or “severely depressed” (LVEF < 30%).25, 28 Additionally, in cardiac arrest patients, one can recognize “no coordinated myocardial activity” as a likely indicator of futility of further resuscitation.29 Hyperdynamic states are typically associated with decreased afterload, and are most commonly found in patients with sepsis or severe hypovolemia. A severely depressed ejection fraction, particularly when paired with a plethoric IVC (and/or B-lines on thoracic images), indicates systolic heart failure.
Techniques for Assessing Ejection Fraction
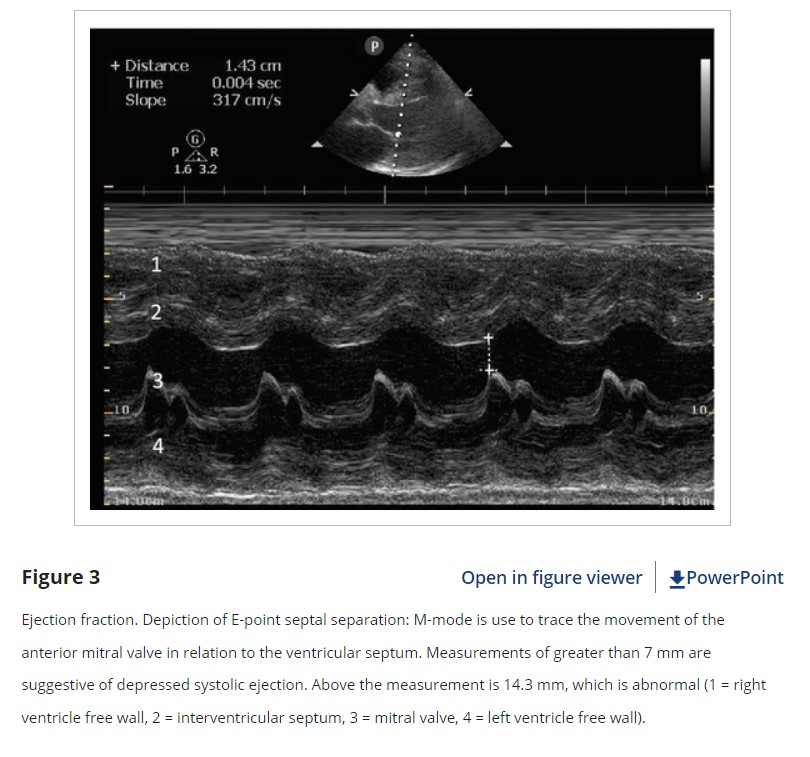
For a visual determination of LVEF, the PSLA view is an excellent initial window. The PSLA includes the septum, apex, and posterior LV wall. Additionally, the PSLA view provides good visualization of the anterior leaflet of the mitral valve, allowing for assessment of E-point septal separation (EPSS). Movement of the anterior leaflet of the mitral valve so that it nearly touches the septum in diastole correlates with good LV filling and thus a good ejection fraction.30 EPSS may be assessed by visual estimation or measured quantitatively using B-mode or M-mode to measure the smallest distance from the anterior mitral valve tip to the septal wall during diastole (Figure 3). EPSS measurements greater than 7 mm have been shown to correlate with severely depressed LVEF.31 Rotating from the PSLA to a PSSA view at the level of the papillary muscles shows the entire circumference of the muscular portion of the LV.32 This is an optimal window to observe the concentric squeeze of the LV by estimating the degree of internal chamber collapse in systole versus diastole. This view is also useful to detect focal wall motion abnormalities. In a PSSA view proceeding in a clockwise direction, the septal, anterior, lateral, posterior, and inferior wall segments of the mid-portion of the LV are visible (mnemonic “SALPI”).
The A4C window also provides a good view of the global function of the myocardium, but should include an apical two-chamber view to evaluate all parts of the myocardium. The subxiphoid views may also provide information about global myocardial function, but it may be difficult to see all portions of the LV.
Pearls and Pitfalls of Ejection Fraction
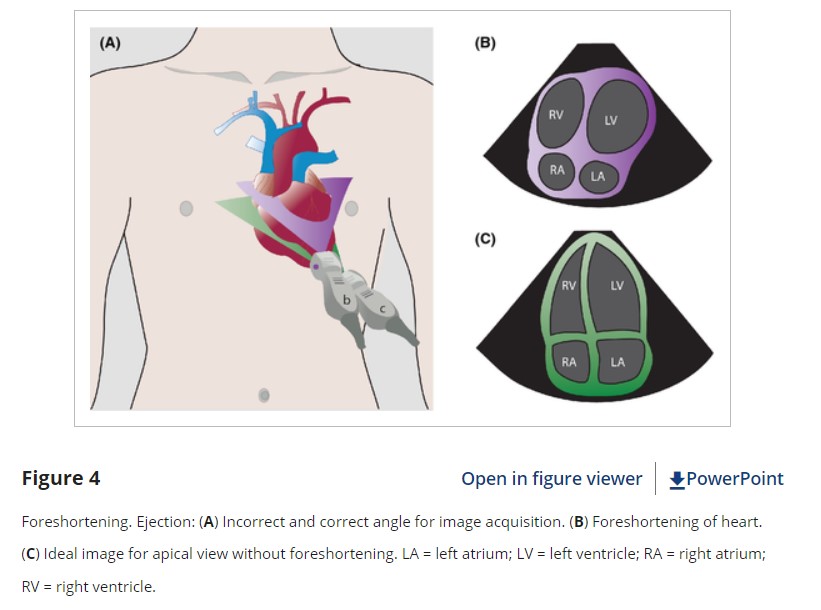
While EPs are very good at distinguishing normal function from severe dysfunction, moderate LV dysfunction can be more difficult to reliably discern.25 It is important to optimize the LV view at the widest diameter of the LV chamber with clearly visible endocardial borders. Being oblique to the LV chamber may underestimate its size and overestimate its emptying (Figure 4). EPSS is a good surrogate measure of ejection fraction, but can be confounded by septal hypertrophy, mitral valve stenosis, or mismeasurements. Two-dimensional images (especially in the A4C view) can be limited by poor lateral resolution and decreased visualization of endocardial borders.31
While the basic EP FOCUS assessment is for estimation of global ejection fraction, focal wall motion abnormalities can affect overall function and represent a pitfall if not appropriately recognized or characterized. Incomplete visualization of all portions of the LV can result in missed focal wall motion abnormalities. When present, these typically indicate myocardial dysfunction or scarring from ischemia, which may be acute or chronic. Myocardial contraction should be observed for several heartbeats, particularly if there are premature ventricular contractions or underlying arrhythmias, such as atrial fibrillation.
Even with a preserved ejection fraction, heart failure still remains a possible cause of dyspnea. Approximately half of all heart failure cases may have some component of impaired relaxation leading to diastolic dysfunction, also known as heart failure with preserved ejection fraction.32
Conclusions
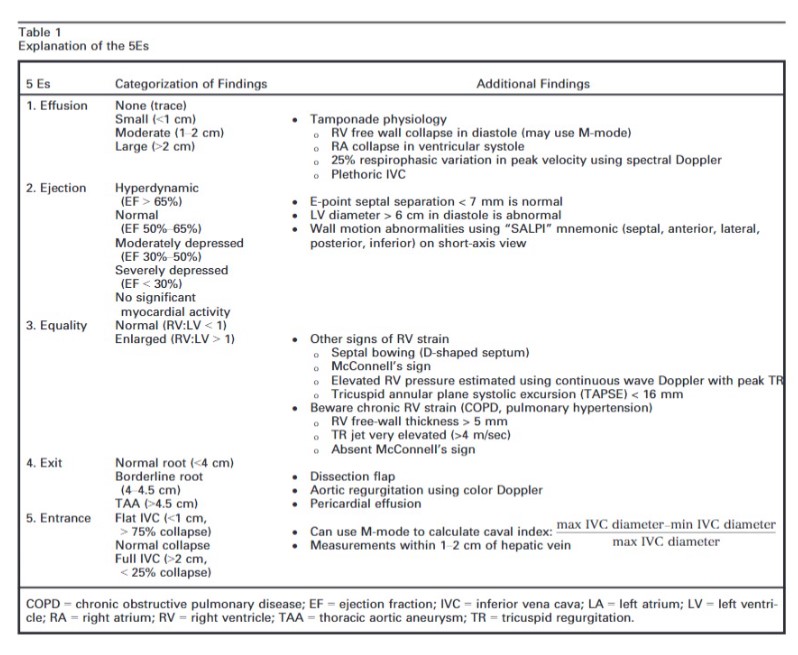
The intent of this article is to codify elements of the cardiac US exam that we have found to be most relevant to patients presenting with acute or emergent complaints (Table 1). A recent international consensus statement defined FOCUS as being goal-directed, problem-oriented, limited in scope, simplified, time-sensitive and repeatable, qualitative and semiquantitative, performed at the point of care, and usually performed by clinicians.6 The 5Es described in this article meet all of these criteria. However, the international statement addressed the use of FOCUS in “all clinical settings” and included the assessment of chronic cardiac disease, as well as gross valvular abnormalities and large intracardiac masses, without assessment of the thoracic aorta.
In our experience the 5Es encompass the cardiac US findings most applicable in patients who present emergently with hypotension, dyspnea, syncope, penetrating thoracic trauma, chest pain, or other acute complaints where diagnosis may be aided by visualization of the heart. While gross valvular abnormalities and intracardiac masses are important if they are seen, they are less common and less acute and tend to be less immediately deadly than acute thoracic aortic disease, which accounts for more than twice as many deaths as abdominal aortic aneurysm rupture.51The 5Es are not meant to provide an absolute boundary for EP FOCUS, which will likely continue to evolve, but are intended to provide a framework for the acquisition and interpretation of the most relevant and applicable components of echocardiography in the emergent setting. We hope that adoption and subsequent application of the 5Es in EDs will help to standardize and effectively teach the echo findings that may allow EPs to save lives and expedite the care of patients with potentially life-threatening illness. We thank Jane Hall, PhD, for preparing Figures 4, 6, and 8. We also thank Daniel Wadsworth Groves, MD, for manuscript review.