This post contains links to and excerpts from ESC Council on hypertension position document on the management of hypertensive emergencies [PubMed Abstract] [Full Text HTML] [Link to the full text PDF is through the Full Text HTML]. Eur Heart J Cardiovasc Pharmacother, 5 (1), 37-46 2019 Jan 1.
Here are excerpts:
Abstract
Hypertensive emergencies are those situations where very high blood pressure (BP) values are associated with acute organ damage, and therefore, require immediate, but careful, BP reduction. The type of acute organ damage is the principal determinant of: (i) the drug of choice, (ii) the target BP, and (iii) the timeframe in which BP should be lowered. Key target organs are the heart, retina, brain, kidneys, and large arteries. Patients who lack acute hypertension-mediated end organ damage do not have a hypertensive emergency and can usually be treated with oral BP-lowering agents and usually discharged after a brief period of observation.
Definitions
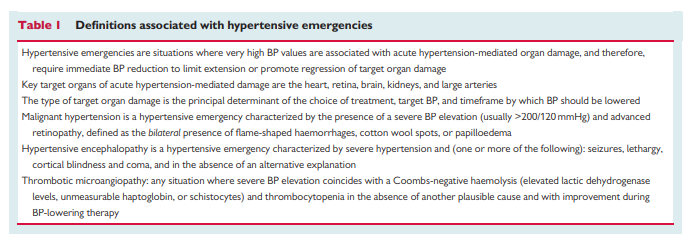
An overview of current definitions used for hypertensive emergencies and associated conditions is given in Table 1
Hypertensive emergencies can be classified according to the presence of acute hypertension-mediated target organ damage.1
In patients with a hypertensive emergency immediate BP reduction is indicated to limit extension or promote regression of acute hypertension-mediated organ damage. The type of target organ damage is the principal determinant of the choice of treatment, target BP, and timeframe by which BP should be lowered.
A typical example of a hypertensive emergency is the coexistence of very high BP values (often >200/ 120 mmHg) with advanced retinopathy, acute renal failure, and/or thrombotic microangiopathy (TMA).
Hypertensive encephalopathy occurs in 10–15% of patients presenting with malignant hypertension. However, advanced hypertensive retinopathy may be lacking in up to one-third of these patients.6 Therefore, the diagnosis principally relies on the presence of neurological symptoms supported by additional imaging. Seizures, lethargy, cortical blindness, and coma are among the most alarming symptoms, but more subtle neurological features can be present at an earlier stage.7
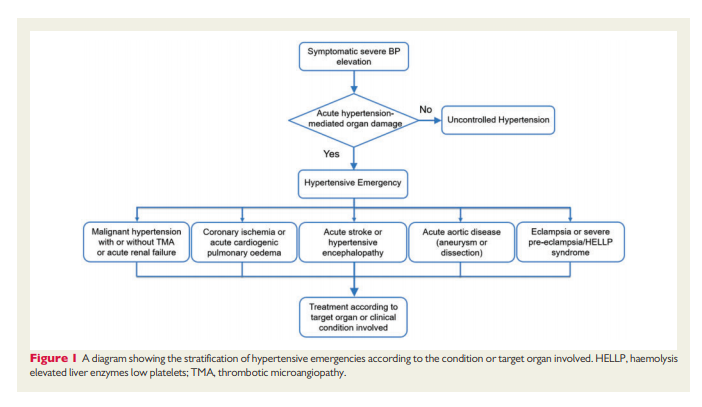
Other examples of hypertensive emergencies are severe
hypertension in patients with intracranial haemorrhage and acute stroke, acute coronary syndrome, cardiogenic pulmonary oedema, acute aortic disease, and severe pre-eclampsia and eclampsia. A diagram showing the stratification of different hypertensive emergencies according to the condition or target organ involved is shown in Figure 1.
Epidemiology
One in every 200 patients presents at the ED with a suspected hypertensive emergency,9 a proportion that has not changed in the past two decades,10 and seems comparable across continents.11–14 Based on current definitions, approximately one in every two to three patients have a hypertensive emergency.9,12,13 In a representative sample of ED visits in the US, heart failure, stroke, and myocardial infarction represented the largest proportion of all hypertensive emergencies, followed by intracranial haemorrhage and aortic dissection, whereas the incidence of hypertensive emergencies with advanced
retinopathy was quite low.13 However, this may relate to differences in categorization as other studies using different coding systems have found much higher incidence rates.14Pathophysiology
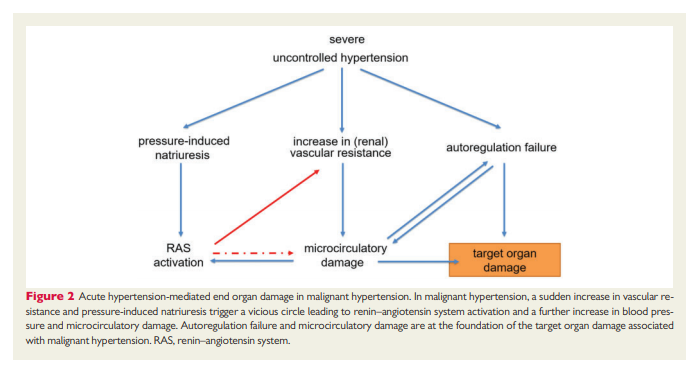
In patients presenting at the ED with malignant hypertension, secondary causes can be found in 20–40% and most oftenconsist of renal parenchymal disease and renal artery stenosis, whereas endocrine causes appear to be rare.15,17 However, the majority of patients with malignant hypertension have unrecognized or uncontrolled essential hypertension. Many pathophysiological mechanisms are involved in the development and maintenance of malignant hypertension (Figure 2), but the initiating events for the sudden escalation in BP are
not completely.
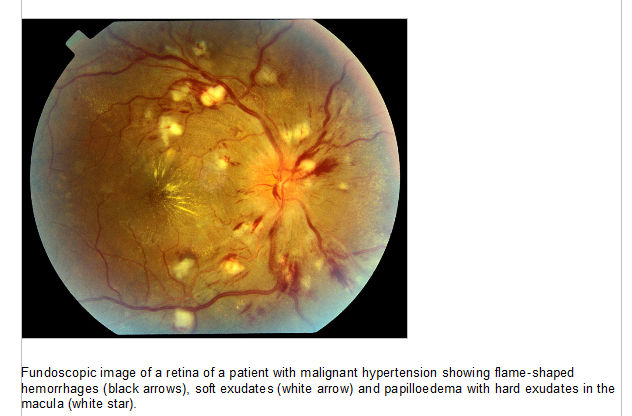
Hypertensive retinopathy
The retinal abnormalities associated with malignant hypertension consist of flame shaped haemorrhages, cotton wool spots (Grade III) with or without the presence of papilloedema (Grade IV). These retinal abnormalities are rare in the normal population and, when they are bilaterally present, highly specific. Because Grade III and IV hypertensive retinopathy have the same pathophysiological background
and carry the same prognosis,23,24 it is justified to stratify patients into those with and without advanced retinopathy. The presence of advanced hypertensive retinopathy in patients presenting at the ED with a suspected hypertensive emergency is associated with much higher renin–angiotensin system activation and more pronounced hypertension-mediated organ damage in other areas compared with patients without these retinal lesions, despite comparable BP values.3A funduscopic image of advanced retinopathy is added as Supplementary material online [included below]
Thrombotic Microangiopathy
Both high BP and angiotensin II have been associated with activation of pro-inflammatory and pro-coagulant pathways.25,26 Endothelial detachment is one of the pathological hallmarks of hypertensive microangiopathy and is thought to result from high-shear forces.
The subsequent exposure of blood to the subendothelium leads to coagulation activation, platelet activation, and the formation of a fibrin network. These result in: (i) the formation of platelet-rich thrombi with obliteration of the microcirculation and (ii) platelet consumption and intravascular haemolysis as a result of trapping and destruction of erythrocytes within the fibrin network.
Discrimination from other causes of TMA such as thrombotic thrombocytopenic purpura (TTP) and haemolytic uraemic syndrome (HUS) can be difficult.*
*See the following resources:
- Links To And Excerpts From “How to Interpret and Pursue an Abnormal Complete Blood Cell Count in Adults” With Additional Resources
Posted on August 20, 2019 by Tom Wade MD - Links To And Excerpts From “Common CBC Abnormalities” From The Curbsiders
Posted on August 20, 2019 by Tom Wade MD - Thrombotic Thrombocytopenic Purpura (TTP)
Updated: Feb 18, 2019 from emedicine.medscape.com
- Hemolytic Uremic Syndrome By Dr. Larry Mellick
Posted on July 28, 2015 by Tom Wade MD - “IBCC chapter & cast: Acute Kidney Injury” – Links And Excerpts
Posted on May 10, 2019 by Tom Wade MD