Note: I originally posted this on Aug 20, 2019. I’m reposting it today, 8-18-2021 because I am reviewing all the resources in the post.
This post contains links to and excerpts from #167 LIVE! Common CBC Abnormalities with Mary Kwok MD
[Link is to the podcast and show notes]. AUGUST 19, 2019 By MATTHEW WATTO, MD from The Curbsiders.
The above podcast is good but I don’t need to review it again. Instead here are excerpts from the show notes that I found helpful:
Initial Approach to common CBC abnormalities
Look at the white count (WBC), Hemoglobin (Hgb), Platelets (Plt), MCV, and the differential (diff).
Next, calculate the absolute counts e.g. absolute neutrophil count, etc. The absolute counts trump the percentages when reviewing a CBC with diff.*
* Always determine if the absolute count of each of the leukocyte types is in the normal range when looking for abnormalities. And make decisions on the next step in evaluation based on the absolute count.
Dr. Kwok [recommends] that an abnormal CBC should [first] be repeated to see if the abnormalities persist.
Leukocytosis
DDX FOR LEUKOCYTOSIS
Smoking and infections commonly cause neutrophilia. Lymphocytosis is suspicious for a lymphoproliferative disorder. Older patients with monocytosis may have CMML.
Smoking is a common cause of neutrophilia. Tell the patient to stop smoking and then repeat the labs.
LEUKOCYTOSIS RED FLAGS
Blasts, elevated basophils (suggests myeloproliferative neoplasm), absolute eosinophil count over 1500, absolute lymphocyte count over 5000 all warrant a hematology consult. These patients may need bone marrow biopsy.
WHAT IS FLOW CYTOMETRY?*
Blood is tagged with markers. Millions of cells are analyzed and plotted on a scatter plot. Then, a pathologist identifies any abnormal populations of cells e.g. clonal B cells, T cells, myeloid blasts, or lymphoid blasts.
*See Use of Flow Cytometry in Clinical Practice [PubMed Abstract] [Full Text HTML] [Full Text PDF]. J Adv Pract Oncol. 2015 Sep-Oct;6(5):435-40. Epub 2015 Sep 1.
The above article is a good basic introduction to flow cytometry.
WHEN SHOULD FLOW CYTOMETRY BE ORDERED?*
- Patient with suspicious lymphadenopathy
- Patient with absolute lymphocyte count over 5000
*My own practice is usually to refer a patient who I believe needs flow cytometry to a hematologist/oncologist for further evaluation.
*Here are two articles that demonstrate why flow cytometry is usually is best ordered by a specialist [The articles below don’t need to be reviewed again – what they do emphasize is that often the next step for the primary care clinician is the peripheral smear reviewed by the laboratory physician]:
- Practical challenges in peripheral blood smear evaluation, March 2019 from CAP Today
- Peripheral blood evaluation: B12 deficiency, anemia, ET, CMML, April 2019 from CAP Today
Leukopenia
INITIAL STEPS
Review previous CBCs to check for chronicity. Review medication exposures to look for culprits. Ask about a history of acute, chronic or recurrent infections. Does the patient have a known rheumatologic disorder?
Check the peripheral smear* to look for blasts or other abnormal cells.
*See the following for information on the peripheral smear:
- Peripheral blood film – a review [PubMed Abstract] [Full Text HTML] [Full Text PDF]. Ann Ib Postgrad Med. 2014 Dec;12(2):71-9.
- This is an awesome brief review of the peripheral smear. Note to myself: Useful to review again and again. And a fast read.
- Clinical Hematology Atlas, 3rd Edition (Spiral-bound)by Jacqueline H. Carr MS CLSpH(NCA) CLDir(NCA), Bernadette F. Rodak MS MLS
- 2009 – there are newer atlases but they are much more expensive.
BENIGN ETHNIC NEUTROPENIA
Benign ethnic neutropenia can be confirmed by checking an RBC phenotype. Patients who are Duffy null (negative for Duffy A and B) likely have benign ethnic neutropenia.
Rheumatologic diseases may be a cause of neutropenia, but they’re usually symptomatic (NOT an occult process).
Erythrocytosis (aka Polycythemia)
Defined as hemoglobin (Hgb) above 16.5 g/dL for a man, or above 16 g/dL for a woman (Tefferi A. UpToDate 2019).
DDX FOR ERYTHROCYTOSIS (POLYCYTHEMIA)
- Myeloproliferative neoplasm (MPN) such as polycythemia vera (PV)
- Renal disease – Cysts, renal artery stenosis, renal cell carcinoma
- Chronic hypoxemia from lung disease, sleep apnea, smoking
- Certain erythropoietin (EPO) producing tumors
WORKUP ERYTHROCYTOSIS
Check for splenomegaly. Repeat the CBC. Next, check an EPO level. A low EPO level suggests a primary process like PV. Consider sending a JAK2 mutation for patients with a low EPO level and clinical suspicion for PV. A normal or elevated EPO level suggests a secondary erythrocytosis from hypoxia, a renal process or EPO secreting tumor.
POLYCYTHEMIA VERA SIGNS AND SYMPTOMS
Aquagenic pruritus is stinging, burning or itching that occurs in response to water exposure. Erythromelalgia is intermittent burning pain (often severe) in hands or lower extremities. It’s believed to be caused by blocked blood vessels.
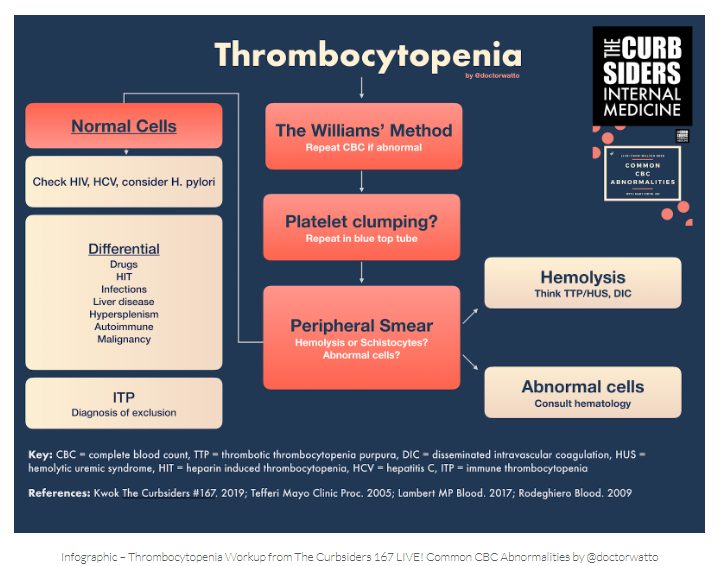
Thrombocytopenia
If the patient has thrombocytopenia and is sick you must consider Disseminated Intravascular Coagulation and Thrombotic Thrombocytopenia. And the very best resources on this topic are from EMCrit [Simply Awesome]:
- EMCrit Podcast 223 – TTP & DIC with Tom DeLoughery – Part I – Diagnosis
April 30, 2018 by Scott WeingartThe best way to watch this vidcast is on YouTube because on your laptop you can follow along by reading the transcript of the lecture that accompanies every YouTube video. I have to be watching on my laptop. I can’t access the transcript on my phone or tablet. - YouTube link for #223
- EMCrit Podcast 224 – TTP & DIC with Tom DeLoughery – Part II – Treatment
May 14, 2018 by Scott WeingartBest to watch the vidcast on YouTube on your laptop-same reason as above. - YouTube Link for #224.
SIMPLIFIED APPROACH TO THROMBOCYTOPENIA
- Is the thrombocytopenia isolated or accompanied by anemia and/or leukopenia?
- Review the patient’s medication list and pay attention to any recent changes or exposures (e.g. antibiotics, chemo, antidepressants). Is there evidence of hemolysis?
- Consider DIC, TTP/HUS, HIT or acute leukemia in patients who look sick.
- Ask about hepatitis C, HIV and if dyspepsia is present, H. pylori infection.
- Decide if the patient is at risk for nutritional deficiencies. Do they have known liver disease (hypersplenism from portal hypertension or decreased production of thrombopoietin), thyroid disease, autoimmune or rheumatologic conditions?
THROMBOCYTOPENIA ANECDOTE
Dr. Kwok has not seen platelets improve much after treating patients for H. pylori.
ISOLATED THROMBOCYTOPENIA
First repeat the CBC. Next, check a peripheral smear. Use a blue top tube to overcome any platelet clumping noted on the smear. Rule out hemolysis (bilirubin, LDH, haptoglobin, +/- direct antiglobulin test). Check HIV, and hepatitis C. Consider sending liver function tests, H. pylori, TSH, HCG (in women), SPEP/UPEP, B12 and folate depending on the clinical history (Tefferi 2005; Lambert 2017)
Immune thrombocytopenia (ITP) is a diagnosis of exclusion.
Resources:
(1) #167 LIVE! Common CBC Abnormalities with Mary Kwok MD [Link is to the podcast and show notes]. AUGUST 19, 2019 By MATTHEW WATTO, MD from The Curbsiders.
(2) How to Interpret and Pursue an Abnormal Complete Blood Cell Count in Adults [PubMed Abstract] [Full Text HTML] [Full Text PDF]. Mayo Clin Proc. 2005. Jul;80(7):923-36.
(3) Hypersplenism: History and current status [PubMed Abstract] [Full Text HTML] [Full Text PDF]. Exp Ther Med. 2016 Oct; 12(4): 2377–2382.
(4) Point-of-care ultrasonography improves the diagnosis of splenomegaly in hospitalized patients [PubMed Abstract] [Full Text HTML] [Full Text PDF]. Crit Ultrasound J. 2015; 7: 13
(5) Approach To Lymphocytosis 2017 from Cancer Therapy Adviser
(6) Evaluation of Patients with Leukocytosis [PubMed Abstract] [Full Text HTML] [Full Text PDF]. Am Fam Physician. 2015 Dec 1;92(11):1004-11.