Note to myself-In addition to today’s resource, please see and review:
- “Postmenopausal Bleeding” From StatPearls
Posted on February 26, 2023 by Tom Wade MD - Linking To And Excerpting From “Diagnostic criteria for nonviable pregnancy early in the first trimester”
Posted on November 15, 2022 by Tom Wade MD - Links To And Excerpts From emDocs’ “Speculations on the Speculum: Is a pelvic exam ever needed in the ED?”
Posted on November 14, 2022 by Tom Wade MD - “False negative point-of-care urine pregnancy tests in an urban academic emergency department: a retrospective cohort study”-Links And-Excerpts
Posted on February 25, 2023 by Tom Wade MD- The Bottom Line: “False negative urine pregnancy tests in the emergency department risk iatrogenic harm as well as delayed diagnosis of pregnancy complications. This retrospective study founda prevalence of 1.6%, including multiple ectopic pregnancies,and a 3.6% rate among females presenting with abdominal pain or vaginal bleeding.
- Reviewing “Ectopic Pregnancy: Diagnosis and Management” From The American Family Physician
Posted on November 15, 2022 by Tom Wade MD
In this post, I link to and excerpt from The Curbsiders’ #382 Abnormal Uterine Bleeding With Dr. Holly Wong Cummings, 57:56, By Dr.
All that follows is from the above resource.
Transcript-382-Uterine-Bleeding.docx
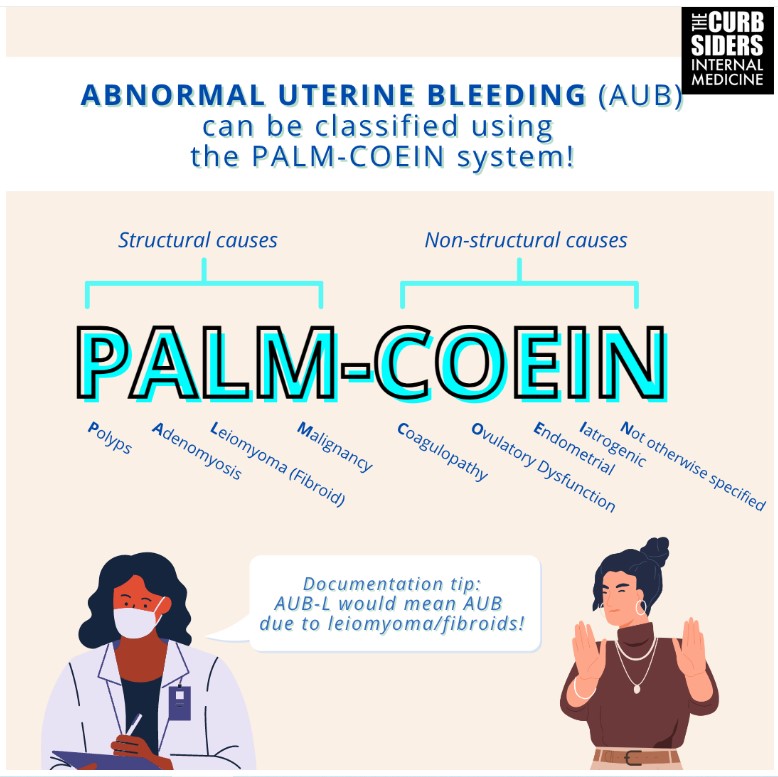
Listen in as we talk through abnormal uterine bleeding (AUB) with our esteemed guest Holly Wong Cummings, MD. We review the PALM-COEIN framework for AUB diagnosis and discuss options for acute and chronic treatment of AUB. We can get bleeding under control! Many of the treatments including progesterone only pills, combined oral contraceptives, and tranexamic acid are medications we in primary care should feel confident prescribing to our patients.
Show Segments
- Intro, disclaimer, guest bio
- Case from Kashlak
- Normal Menstrual Cycle
- Nomenclature for AUB- PALM COEIN
- History and Physical Exam
- Laboratory and radiologic evaluation
- Structural causes for bleeding/interpreting the ultrasound
- Acute treatment of AUB
- When to refer to ED
- Chronic treatment for AUB
- When to refer to gyn
- Take home points
- Outro
Abnormal Uterine Bleeding Pearls
- Use the PALM-COEIN framework both to help you with your differential for AUB as well as to be able to communicate with others around the patients’ diagnosis.
- Physical exam is important in AUB. Primary care providers and internists should appreciate the value of performing pelvic examinations.
- For most patients with AUB, checking a CBC and TSH is reasonable/appropriate.
- The pelvic ultrasound is the most valuable test for determining the cause of AUB.
- Treating acute AUB with either a progesterone alone (ie norethindrone), a combined oral contraceptive pill, or tranexamic acid is effective and should be tailored to patients medical contraindications to estrogen therapies and/or preferences around use of daily vs episodic medication.
- For long term treatment of AUB, continuation of acute treatments described above, LARCs like the levonorgestrel IUD or etonogestrel arm implant, or referral to gyn for surgical therapies such as endometrial ablation, myomectomy, or hysterectomy are appropriate options.
Abnormal Uterine Bleeding Notes
Normal Menstrual Cycle
Cycle day 1 of the menstrual cycle is the first day of bleeding. Typical bleeding lasts 5-7 days. Ovulation occurs typically at day 12-14. If fertilization does not occur, then typically around day 27-28, the endometrium starts shedding and the cycle restarts. There is a complex interplay between hormones from the hypothalamus to pituitary to ovaries to trigger ovulation and the build up and shedding of the endometrial lining.
Nomenclature for AUB:
FIGO (International Federation of Gynecology and Obstetrics) suggests a standard nomenclature around AUB (abnormal uterine bleeding). Calling this dysfunctional uterine bleeding (DUB) and terms like metrorrhagia or menometrorrhagia are currently discouraged. Menorrhagia is still commonly used to describe heavy menstrual bleeding, but the FIGO preferred term is just “heavy menstrual periods”.
PALM COEIN
Structural causes:
P: Polyps
A: Adenomyosis
L: Leiomyoma (fibroid)
M: Malignancy (or premalignancy/hyperplasia)
Nonstructrual causes
C: coagulopathy
0: ovulatory dysfunction (PCOS, etc)
E: endometrial (chronic endometritis)
I: iatrogenic (anticoagulation, hormonal contraceptives, etc)
N: not otherwise specified.
Documentation can then briefly explain the situation- ie AUB-L means abnormal bleeding due to fibroids (Munro 2011).
We have had 2 other great curbsiders episodes covering PCOS (#198) and menorrhagia due to coagulopathy (#280) if you want to learn more about AUB-C, O, and I.
History
Dr Cummings likes to confirm with the patient that they are counting their days in a standard way- sometimes patients count the day from stopping bleeding to when they start again, instead of from start to next start. She also likes to get an understanding of their prior cycle history: are there months where the patient is not bleeding at all during a cycle or bleeding in between cycles/intermenstrual bleeding? She also suggests asking about plans around pregnancy.
Physical Exam
ACP does not recommend routine bimanual exams (Qaseem 2014), but Dr Cummings points out that when a patient presents with abnormal bleeding, this is not a screening/routine exam anymore. On abdominal exam, sometimes large fibroids can be palpated. Speculum exam can help you see gross abnormalities on the cervix. The bimanual exam can help determine the size of the uterus. Dr Cummings encourages primary care providers and internists to feel comfortable building their skills around pelvic exams.*
*However, please see Links To And Excerpts From emDocs’ “Speculations on the Speculum: Is a pelvic exam ever needed in the ED?”
Posted on November 14, 2022 by Tom Wade MD. But a speculum exam can still be necessary to visualize the cervix in vaginal bleeding.
Testing
LABS
It is not unreasonable to check a blood count, to rule out anemia. TSH is valuable as thyroid dysfunction can cause abnormal bleeding. Ruling out pregnancy is important (Wouk 2019).*
*See “False negative point-of-care urine pregnancy tests in an urban academic emergency department: a retrospective cohort study”-Links And-Excerpts
Posted on February 25, 2023 by Tom Wade MD
-
- The Bottom Line: “False negative urine pregnancy tests in the emergency department risk iatrogenic harm as well as delayed diagnosis of pregnancy complications. This retrospective study founda prevalence of 1.6%, including multiple ectopic pregnancies,and a 3.6% rate among females presenting with abdominal pain or vaginal bleeding.
PELVIC ULTRASOUND
A pelvic ultrasound [meaning both atransabdominal and transcervical] is a standard part of the evaluation for AUB. Checking this in the follicular phase (after the heaviest bleeding has stopped and before ovulation, when the endometrial lining is thinnest) can be most helpful, but you should not limit getting the ultrasound done at other times in the cycle if scheduling is a challenge. Dr Cummings does suggest it’s reasonable to defer the ultrasound if you are planning to just start treatment, knowing you can consider checking it in the future.
SONOHYSTEROGRAPHY
This test involves a saline infusion through a cervical catheter into the uterus. Simultaneous ultrasound can image the saline infuse through the uterine cavity and into the fallopian tubes, allowing for a detailed image of the inner uterine cavity. These are only available in some centers, and in Dr Cummings’ experience not used frequently (ACOG 2012).
HYSTEROSALPINGOGRAM
A hysterosalpingogram involves injecting dye into the uterus through the cervix under fluoroscopic imaging to assess the passage of dye into the fallopian tubes. This test is primarily for tubal patency, but can sometimes also reveal details about the endometrial cavity. In general this is more commonly used for fertility evaluation than in evaluation for AUB.
ENDOMETRIAL BIOPSY
ACOG guidelines suggest in patients over age 45 with AUB, it is appropriate to get an endometrial biopsy (EMB), and consider biopsy in a younger patient with AUB who has risk factors for endometrial hyperplasia such as unopposed estrogen exposure. Dr Cummings finds shared decision making especially important in these situations. She suggests allowing the patient to decide if and when they are ready to have the EMB (with ibuprofen before hand, and being emotionally prepared). An alternative might be a D+C (dilation and curettage) in the operating room if someone is unable to tolerate an in office biopsy. Dr Cummings agrees because abnormal uterine bleeding is so common in patients with a uterus around perimenopause, many patients can qualify for an EMB.
Dr Cummings approach is that many times patients with AUB who are eligible for EMB are given progesterone as part of their treatment plan, so she is less concerned about missing endometrial hyperplasia as progesterone is a treatment for endometrial hyperplasia, or sometimes even early endometrial cancers. Progesterone is protective for the endometrial lining (Gompel 2020).
CERVICAL EVALUATION
Sometimes it can be difficult to differentiate cervical bleeding from uterine bleeding just on history. Dr Cummings suggests it may be reasonable to get a “diagnostic” pap test, even if someone is up to date on cervical cancer screening, as sometimes vaginal bleeding is not actually uterine bleeding, and we should rule out cervical problems as the cause for bleeding.
Structural Causes for AUB: Ultrasound Findings
Fibroids
Fibroids are very common; 65-75% of people with a uterus may have a fibroid. These can range from very small (1cm or less) on today’s detailed imaging to people with fibroids so big they rival a full term pregnancy. Dr Cummings considers a 4-5 cm fibroid small. Potentially all fibroids can contribute to heavier periods, regardless of size or location. Fibroids can be pedunculated (hanging off the outside of the uterus), subserosal (within the uterine muscle layer), or submucosal (intracavitary). Submucosal fibroids may contribute more to heavy bleeding.
Fibroids can be managed hormonally with oral medications or IUDs. Referral to gynecology can be helpful if a patient is interested in considering surgical options (Whitaker 2015).
Adenomyosis
The endometrial cells are within the muscle layer of the uterus instead of being contained within the uterine cavity. When the lining cells bleed and shed, the endometrial cells within the muscle also bleed and attempt to shed, causing painful and heavy periods (Bourdon 2021).
Endometrial Thickness
In a postmenopausal patient (>1 year without menses) who presents with bleeding, an ultrasound measured endometrial thickness > or equal to 5mm warrants further evaluation (ACOG 2018).
In a menstruating patient, the endometrial lining will wax and wane significantly through the cycle, there is no specific number that would be concerning. Dr Cummings suggests that the endometrial stripe can be helpful in predicting ongoing bleeding in the short term- if the endometrial stripe is still thick, the patient likely has significant bleeding ahead. If the endometrial lining is 2mm, the patient is likely close to being done bleeding.