In this post I link to and excerpt from the chapter, Anion-Gap Metabolic Acidosis, September 17, 2019, of Dr. Farkas’ incredible Internet Book Of Critical Care [Link is to TOC]. And after reviewing the chapter, listen to the 13 minute summary podcast of the chapter.
The mnemonic Drs. Farkas and Thomas suggest for anion-gap metabolic acidosis is one I wasn’t familiar with-KULT:
Ketoacidosis (Links below are to emedicine.medscape.com articles on the topics)
Uremia
- Occurs when GFR <20-30 ml/min.
- Uncomplicated uremia rarely causes bicarbonate to fall below ~12-15 mM or anion gap to increase over >20 mM (if these are found, look for an alternative or additional disease process).
Lactic Acidosis
- Inadequate oxygen delivery (“type A hyperlactatemia”)
- Adequate oxygen delivery (“type B hyperlactatemia”)
Toxins (and Medications)
Dr. Farkas has created this Table of Contents of the chapter and each heading is a direct link to that part of the chapter:
CONTENTS
All that follows are excerpts from the Anion-Gap Metabolic Acidosis Chapter of The Internet Book Of Critical Care [except where noted – material in brackets]:
Pitfalls*
[*This section is at the end of the chapter, but also reminds me of why we care.]
- Elevated anion gap should be regarded as reflecting a life-threatening abnormality until proven otherwise. In an ill patient, seriously consider whether elevated anion gap may reflect hyperlactatemia and consider initiating the evaluation for hyperlactatemia (even before the lactate level returns).
- When facing an elevated lactate of unclear etiology, consider empiric IV thiamine. Thiamine deficiency is common in critical illness, and thiamine administration is entirely safe.
- Don’t panic in response to an elevated lactate value following a generalized seizure. This is generally benign and should clear within about an hour – follow closely to ensure that the patient is improving.
- Don’t assume that lactic acidosis indicates the presence of septic shock. Lactic acidosis has an extensive differential diagnosis which includes dozens of disorders (including every type of shock).
Going further:
- iSepsis: The lactate myths also Understanding Lactate (Paul Marik)
- Understanding lactate and using it to our advantage (PulmCrit)
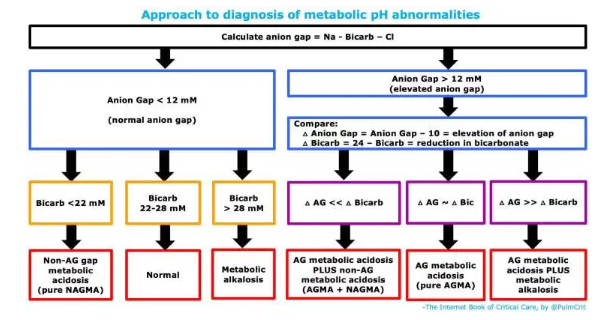
diagnosis
- Anion gap should be evaluated on every electrolyte panel. Ideally the computer will do this automatically; otherwise, it should be calculated.
- Anion gap is calculated as (Na – Cl – Bicarb). Nothing fancy, no corrections for anything (glucose, albumin, potassium, etc.).
- More discussion of the anion gap in the chapter on diagnosing acid/base problems here.
- Elevated anion gap is concerning, because many causes of this are immediately life-threatening.
- (Unlike, for example, non-anion-gap metabolic acidosis – where most causes are not life threats).
causes of elevated anion gap
ketoacidosis
- Diabetic ketoacidosis (DKA)
- Alcoholic ketoacidosis (AKA)
- Starvation ketoacidosis
uremic acidosis
- Occurs when GFR <20-30 ml/min.
- Uncomplicated uremia rarely causes bicarbonate to fall below ~12-15 mM or anion gap to increase over >20 mM (if these are found, look for an alternative or additional disease process).
hyperlactatemia
- Inadequate oxygen delivery (“type A hyperlactatemia”)
- Profound shock
- Regional hypoperfusion: ischemic limb, mesenteric ischemia
- Muscle hyperactivity: seizure, extreme exertion
- Extreme anemia or hypoxemia
- Adequate oxygen delivery (“type B hyperlactatemia”)
- Liver failure
- Malignancy (usually leukemia/lymphoma)
- Thiamine deficiency (e.g. due to persistent critical illness, poor nutritional status, or gastric bypass surgery)
- Beta-2 receptor stimulation
- Exogenous administration of epinephrine, albuterol, or terbutaline
- Endogenous epinephrine secretion (including any type of shock – including septic, cardiogenic, obstructive, or hypovolemic; pheochromocytoma)
- Lactic alkalosis
- Severe diabetic ketoacidosis (DKA)
- Medications
- Beta-agonist excess (e.g. epinephrine, albuterol, terbutaline)
- Linezolid
- Metformin
- Nucleoside reverse-transcriptase inhibitors (e.g. used for treatment of HCV or HIV)
- Propofol (propofol infusion syndrome)
- Propylene glycol intoxication (e.g. due to high intravenous doses of lorazepam, diazepam, nitroglycerine, esmolol, phenytoin)
- Nitroprusside (due to cyanide accumulation)
- Valproic acid, topiramate
- Poisoning
- Acetaminophen poisoning, massive
- Alcohols
- Ethylene glycol (some assays will mis-identify glycolic acid as lactic acid)(31418093)
- Methanol
- Ethanol poisoning (31474479)
- Cyanide, Carbon monoxide
- Salicylate
- Sympathomimetics (cocaine, amphetamine, cathinones)
- Toluene
- Iron
other causes of elevated anion gap
- Hyperphosphatemia
- Metabolic alkalosis (increases the negative charge on albumin)
- D-hyperlactatemia (rare, due to bacterial fermentation following small intestine resection)
- Some medications: colchicine, NSAIDs, high-dose penicillins.
- Poisonings:
- Salicylate
- Ethylene glycol, methanol
- Pyroglutamic acidosis (acetaminophen use)
evaluation & treatment of lactate elevation
#1) consider the differential diagnosis
- Inadequate oxygen delivery (“type A hyperlactatemia”)
- Profound shock
- Regional hypoperfusion: ischemic limb, mesenteric ischemia
- Muscle hyperactivity: seizure, extreme exertion
- Extreme anemia or hypoxemia
- Adequate oxygen delivery (“type B hyperlactatemia”)
- Liver failure
- Malignancy (usually leukemia/lymphoma)
- Thiamine deficiency (e.g. due to persistent critical illness, poor nutritional status, or gastric bypass surgery)
- Beta-2 receptor stimulation
- Exogenous administration of epinephrine, albuterol, or terbutaline
- Endogenous epinephrine secretion (including any type of shock – including septic, cardiogenic, obstructive, or hypovolemic; pheochromocytoma)
- Lactic alkalosis
- Severe diabetic ketoacidosis (DKA)
- Medications
- Beta-agonist excess (e.g. epinephrine, albuterol, terbutaline)
- Linezolid
- Metformin
- Nucleoside reverse-transcriptase inhibitors (e.g. used for treatment of HCV or HIV)
- Propofol (propofol infusion syndrome)
- Propylene glycol intoxication (e.g. due to high intravenous doses of lorazepam, diazepam, nitroglycerine, esmolol, phenytoin)
- Nitroprusside (due to cyanide accumulation)
- Valproic acid, topiramate
- Poisoning
- Acetaminophen poisoning, massive
- Alcohols
- Ethylene glycol (some assays will mis-identify glycolic acid as lactic acid)(31418093)
- Methanol
- Ethanol poisoning (31474479)
- Cyanide, Carbon monoxide
- Salicylate
- Sympathomimetics (cocaine, amphetamine, cathinones)
- Toluene
- Iron
Consider the causes of hyperlactatemia (listed above) within the patient’s clinical context. Hyperlactatemia may occur in shock due to any etiology, so if there are features of shock then resuscitation should begin without delay (more on the evaluation of undifferentiated shock here).
#2) review medications
- Make particularly sure to review the patient’s medication list, with attention to medications which can elevate lactate levels (listed above).
- Any medication which could be causing acidosis should be stopped immediately (especially: propofol, nitroprusside, or metformin).
- One potential exception here is hyperlactatemia due to epinephrine. This is not necessarily harmful, in fact some evidence suggests that it may be beneficial (20016405). Unless the lactate elevation due to epinephrine is substantial (e.g. >10 mM), it may be best to continue epinephrine regardless of an elevated lactate level.
#3) send a lab panel
- Repeat lactate level and electrolytes (if there is any doubt about the validity of these labs).
- Note: Occasionally, elevated lactate measurement may result from lab measurement upstream from an infusion of lactated ringers!
- Venous lactate is fine for clinical use. (Technically, arterial lactate is the reference standard. However, venous values are extremely close and clinical decisions should not be made on the basis of small differences in lactate anyway.)
- Complete blood count (if not recently available)
- Elevated white blood cell count or neutrophil/lymphocyte ratio* may reflect systemic illness, such as sepsis.
- [*PulmCrit: Neutrophil-Lymphocyte Ratio (NLR): Free upgrade to your WBC
May 23, 2019 by Josh Farkas]- Severe anemia can increase lactate (but it needs to be extreme).
- Liver function tests (hepatic insufficiency may directly cause or amplify lactate levels).
- Poisoned patient: evaluate for salicylates, acetaminophen, carbon monoxide, and toxic alcohols.
#4) examination
- Signs of shock? (tachycardia, low urine output, hypotension, confusion).
- Signs of focal ischemia? (abdominal pain or cold limb)
#5) treatment of elevated lactate level
- (a) Treat any identifiable causes of hyperlactatemia.
- (b) Empiric IV thiamine repletion if deficiency is possible.
- Thiamine deficiency may be more common than generally believed, particularly among critically ill patients who have been in the ICU for a while.
- It’s impossible to test for thiamine deficiency. When in doubt, just give empiric thiamine (e.g. perhaps ~200 mg IV q12hr).
- (c) Dialysis is generally ineffective (En vivo, lactic acid is very rapidly being produced and metabolized. Dialysis isn’t able to remove lactate rapidly enough to affect this balance).
- (d) Review medication list and discontinue potentially causative medications.
- (e) There is no evidence-based role for bicarbonate in the treatment of elevated lactate level.
treatment
The most important treatment of anion-gap metabolic acidosis is the reversal of its cause. This will vary depending on the etiology.*
bicarbonate
- Uremic AGMA
- Traditionally, bicarbonate has been used to support the pH in efforts to stave off dialysis.
- The BICAR-ICU trial supported the concept of using bicarbonate in uremic metabolic acidosis (with a goal of reducing the requirement for dialysis).
- Other causes of AGMA (e.g. hyperlactatemia or diabetic ketoacidosis)
- Bicarbonate has no evidence-based role here (regardless of pH).
hemodialysis
- May be indicated in patients with metabolic acidosis and renal failure (especially in the presence of volume overload, which precludes the use of IV bicarbonate).
- The exact point at which dialysis is beneficial is controversial (i.e. early dialysis vs. late dialysis).
- According to French guidelines, refractory acidemia (e.g. pH < 7.15 despite conservative measures) might be an indication for dialysis (31418093). However, the overall clinical picture may be more illuminative than any specific cutoff value.
- Earlier dialysis may be indicated for specific intoxications (e.g. metformin, ethylene glycol, methanol, or salicylate). This will be explored in specific chapters on these intoxications.
compensatory hyperventilation
- For intubated patients with mechanical ventilation, it may be reasonable to target a lower pCO2 target than usual.
- The goal here is to mimic the normal physiology of compensatory respiratory alkalosis (a responsibility which the clinician has taken over from the patient’s medulla).
- The extent of hyperventilation will depend on balancing various physiologic derangements:
- In patients with ARDS or obstructive lung disease, achieving a low pCO2 may be impossible or dangerous.
- In patients with severe metabolic acidosis and hemodynamic instability, there may be a greater incentive to improve the pH by decreasing the pCO2. Alternatively, if the acidosis is well tolerated clinically then there is less imperative to adjust the ventilator.
Pitfalls
- Elevated anion gap should be regarded as reflecting a life-threatening abnormality until proven otherwise. In an ill patient, seriously consider whether elevated anion gap may reflect hyperlactatemia and consider initiating the evaluation for hyperlactatemia (even before the lactate level returns).
- When facing an elevated lactate of unclear etiology, consider empiric IV thiamine. Thiamine deficiency is common in critical illness, and thiamine administration is entirely safe.
- Don’t panic in response to an elevated lactate value following a generalized seizure. This is generally benign and should clear within about an hour – follow closely to ensure that the patient is improving.
- Don’t assume that lactic acidosis indicates the presence of septic shock. Lactic acidosis has an extensive differential diagnosis which includes dozens of disorders (including every type of shock).
Going further:
- iSepsis: The lactate myths also Understanding Lactate (Paul Marik)
- Understanding lactate and using it to our advantage (PulmCrit)