What follows is interesting and it may be useful in test taking. But the bottom line is this: If you have failed to get your patient to target blood pressure goals despite your and your patient’s best efforts, refer the patient to an endocrinologist or other hypertension specialist.
As SPRINT has told us blood pressure control is life saving and brain saving.
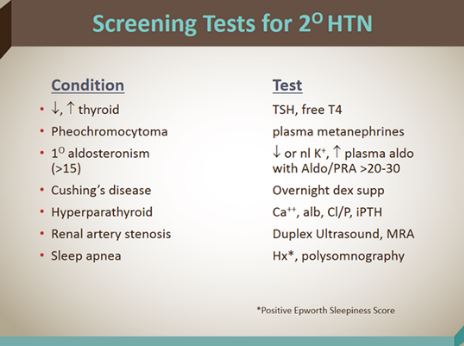
The following slide is from Reference (1) below:
Evaluation for Primary Hypersteronism from Reference (2) in Resources
Here are some brief excerpts from that article:
The term primary hyperaldosteronism (or primary aldosteronism [PA]) refers to a renin-independent increase in the secretion of aldosterone. This condition is principally a disease of adulthood, with its peak incidence in the fourth to sixth decades of life.
Approximately 99% of cases of PA are due either to an aldosterone-producing adenoma (APA), which accounts for around 40% of cases, or due to idiopathic hyperaldosteronism (IHA), which accounts for around 60% of cases (almost all of which are bilateral). About 1% of patients present with adrenocortical carcinomas that are purely aldosterone-secreting and are usually large at the time of diagnosis; 1% present with familial hyperaldosteronism; and, 1% present with an ectopic aldosterone-producing adenoma or carcinoma.[1]
Inherited forms of primary hyperaldosteronism account for only 1% of cases but are more likely to occur during childhood years. These forms include familial hyperaldosteronism (FH) types I, II, and III.
Secondary hyperaldosteronism
Secondary hyperaldosteronism is a collective term for a diverse group of disorders characterized by physiologic activation of the renin-angiotensin-aldosterone (R-A-A) axis as a homeostatic mechanism designed to maintain serum electrolyte concentrations or fluid volume. In the presence of normal renal function, it may lead to hypokalemia.Secondary hyperaldosteronism can be divided into 2 categories, 1 with associated hypertension and 1 without. The former category includes renovascular hypertension, which results from renal ischemia and hypoperfusion leading to activation of the R-A-A axis. The most common causes of renal artery stenosis in children are fibromuscular hyperplasia and neurofibromatosis. Hypokalemia may occur in as many as 20% of patients.
The main complications of primary hyperaldosteronism are hypertension and hypokalemia.
Evaluation of a patient in whom hyperaldosteronism is suggested has several distinct stages. The finding of hypertension, hypokalemia, or both most commonly precipitates the decision to screen. The presence of these 2 features together has a 50% predictive value.
Screening for PA is recommended for patients with Joint National Commission (JNC) stage 2 (>160–179/100–109 mm Hg), stage 3 (>180/110 mm Hg), or drug-resistant hypertension (defined as systolic BP >140 and diastolic BP >90 despite treatment with 3 hypertensive medications); hypertension and spontaneous or diuretic-induced hypokalemia; hypertension with adrenal incidentaloma; or hypertension and a family history of early onset hypertension or cerebrovascular accident at a young age (< 40 y); and all hypertensive first-degree relatives of patients with PA. Additionally, in patients younger than 20 years or those with a family history of PA or stroke at a young age (< 40 y), or with an onset at a young age (eg, < 20 y), genetic testing for glucocorticoid-remediable aldosteronism is suggested.[19, 22]
The first step in the workup entails confirming that hyperaldosteronism is present and, if it is not present, excluding other conditions that produce a similar picture. The next step involves differentiating primary causes of hyperaldosteronism from secondary causes.
Aldosterone-to-renin ratio – This link has detailed information on the test.
The aldosterone-to-renin ratio (ARR)—that is, the ratio of plasma aldosterone (expressed in ng/dL) to plasma renin activity (PRA, expressed in ng/mL/h)—is the most sensitive means of differentiating primary from secondary causes of hyperaldosteronism. It can be obtained under random conditions of sodium intake.
Most of the hyperaldosteronism observed in the general population is sporadic, with most cases due to bilateral adrenal hyperplasia. APAs are likely to be diagnosed earlier than IHA because they are more likely than IHA to produce early symptomatic hypertension and hypokalemia. APAs account for 40% of cases of primary hyperaldosteronism.
It is possible that the distinction between adenoma and hyperplasia is not as clear as was once assumed. In one third of cases, associated hyperplasia or nodules of the adjacent zona glomerulosa is present, implying that the adenoma may have arisen in previously hyperplastic tissue.
Inherited forms of primary hyperaldosteronism (ie, FH-I [GRA], FH-II, and a very rare form known as FH type III [FH-III]) account for approximately 1% of cases of primary hyperaldosteronism, though they are more likely to occur during childhood and adolescent years than other forms of primary hyperaldosteronism are.
Studies of secondary hyperaldosteronism have found that approximately 15% of adults who attend hypertension clinics have elevated PRA. Reliable figures for children are not readily available.
Resources:
(1) Hypertension 2015: Important Concepts in BP Control CME 12-15-2015 fromMedscape
(2) Hyperaldosteronism 12-10-2015 from Medscape