In this post, I link to and excerpt from the six-page PDF, DIAGNOSING AND TREATING MYALGIC ENCEPHALOMYELITIS/CHRONIC FATIGUE SYNDROME (ME/CFS)–U.S. ME/CFS CLINICIAN COALITION –Version 2, July 2020
All that follows is from the above resource.
About the U.S. ME/CFS Clinician Coalition
The U.S. ME/CFS Clinician Coalition is a group of US clinical disease experts who have collectivelyspent hundreds of years treating many thousands of ME/CFS patients. They have authored primers on clinical management, have served on CDC medical education initiatives, and are actively involved in
ME/CFS research.For clinicians who want more information, please contact us through our website (mecfscliniciancoalition.org)
DIAGNOSING ME/CFS
Myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) is a complex, chronic, debilitating disease that affects millions of people worldwide but is often undiagnosed or misdiagnosed. To improve diagnosis, the National Academy of Medicine (NAM) established new evidence-based clinical diagnostic criteria in 2015.PRESENTATION AND RECOGNIZING THE DISTINCTIVE SYMPTOMS OF ME/CFS
The onset of ME/CFS is often sudden. Frequently, patients report that an infectious-like syndrome or infectious disease (such as infectious mononucleosis or flu-like illness) preceded the onset of their disease. Diagnosis requires a thorough medical history, a physical exam, and recognition of the following
core symptoms:➢ Substantial reduction or impairment in the ability to engage in pre-illness activity that persists for 6 months or more and is accompanied by fatigue. The fatigue is profound, not lifelong, not the result of ongoing exertion, and not alleviated by rest.
➢ Post-exertional malaise (PEM) in which physical or mental activities result in a typically delayed and prolonged exacerbation of symptoms and reduction in functioning (discussed further below).
➢ Unrefreshing sleep and a variety of sleep disturbances
➢ Either cognitive impairment (often referred to as “brain fog” by patients) and/or orthostatic intolerance (the development of symptoms when upright that are alleviated when lying down)These core features of illness must be moderate to severe and present at least 50% of the time; this is key to separating ME/CFS from other common causes of chronic fatigue. PEM is the clinical hallmark of ME/CFS and its most distinctive symptom. PEM can help differentiate ME/CFS from other conditions and has been objectively associated with impaired aerobic energy metabolism and orthostatic stress.
Other ME/CFS symptoms include widespread pain; headaches; additional forms of sleep disturbance; visual disturbances; sensitivities to light, noise, chemicals, foods, and drugs; flu-like symptoms including sore throat and tender lymph nodes; susceptibility to infections; gastrointestinal problems; genitourinary issues; respiratory issues such as air hunger; and thermoregulatory issues. The NAM Clinician’s Guide
provides further explanation and guidance on how to identify both core symptoms and additional symptoms. Disease experts may also use the 2003 ME/CFS Canadian Consensus Criteria or the 2011 International Consensus Criteria to validate the diagnosis. (See references for more information).IDENTIFYING THE HALLMARK POST-EXERTIONAL MALAISE (PEM)
Patients experiencing PEM will often describe a “crash,” “relapse,” or “collapse” after even small amounts of mental or physical exertion that was previously tolerated. During the crash, which may be immediate but more often delayed by hours or days, patients can experience an exacerbation of one or all of their symptoms and a further reduction in functioning. It can take hours, days, a week or even longer to return to their previous baseline after a crash. Some patients may go through cycles of overexerting and crashing while others may have learned to reduce or change activities to minimize crashes. For some patients, even basic activities of daily living can result in PEM.The following questions may help identify whether a patient experiences PEM:
● What happens when you engage in normal (previously tolerated) physical or mental exertion?
● How much activity does it take to make you feel ill or to trigger illness worsening?
● How long does it take to recover from this physical or mental effort?
● Do you avoid or change certain activities because of what happens after you do them?It may help patients and clinicians to identify PEM if patients keep a daily diary of their symptoms and activities for two weeks.
DIAGNOSTIC TESTS
While research studies have demonstrated numerous differences in biological measurements in ME/CFS, there is not yet a test validated for the diagnosis of ME/CFS in clinical practice. But there are many diagnostic tests to help identify other fatiguing illnesses or comorbid conditions that are often found in
people with ME/CFS. For example, orthostatic intolerance can be assessed with a NASA Lean Test (standing test) or a tilt table test for 10-20 minutes or up to 30 minutes for neurally mediated hypotension (see Rowe 2014). Beyond helping to establish a diagnosis, tests can also be important in developing
treatment plans to address comorbid conditions. Disease experts may also use lab tests to identify issues such as immune impairment to guide treatment but these are more typically used by specialists and in research.THE IMPORTANCE OF DIFFERENTIAL DIAGNOSIS
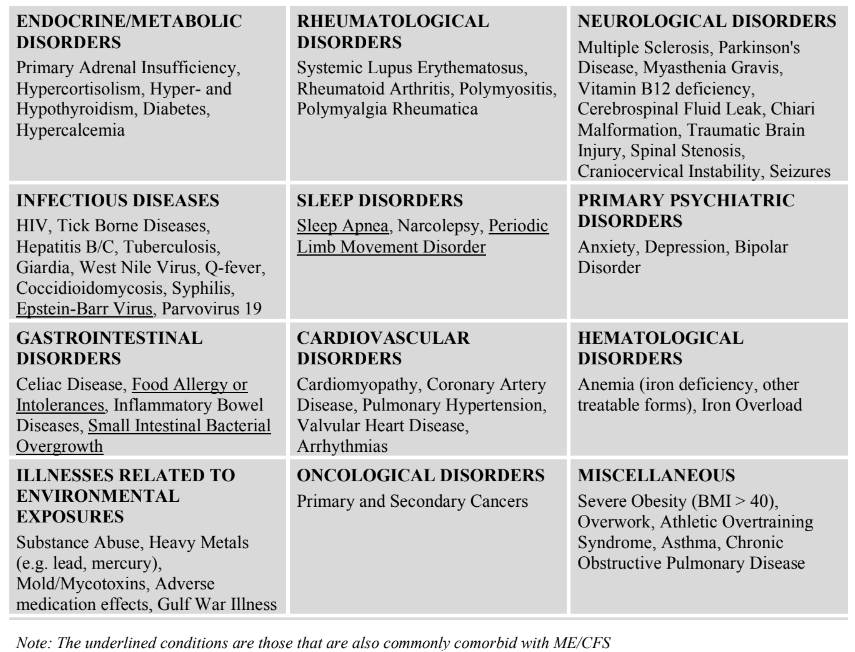
Some of the symptoms of ME/CFS are also observed in healthy people as well as people affected by other
illnesses. Appropriate treatment of these other conditions may completely resolve the patient’s symptoms.
Thus, it is important to distinguish between ME/CFS and these other conditions. Important diseases in this
category include but are not limited to the following:IDENTIFYING COMMONLY COMORBID CONDITIONS
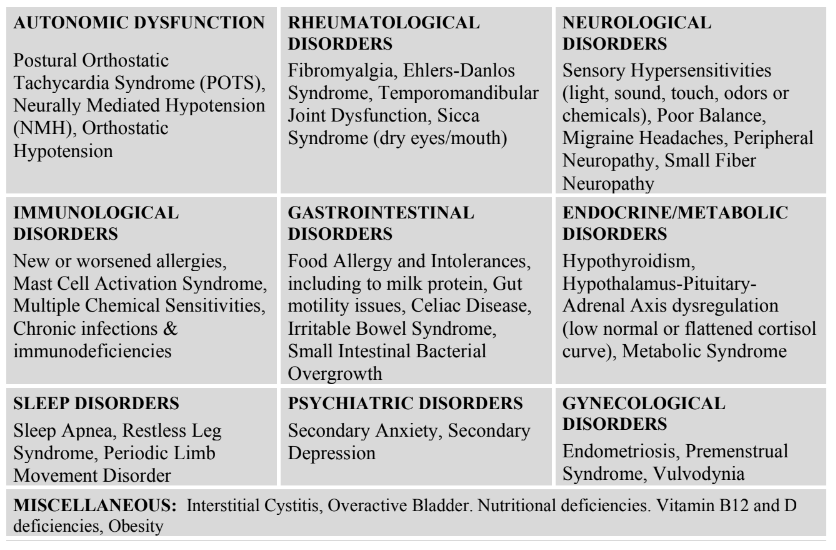
In the past, a diagnosis of ME/CFS was made by first excluding all other possible conditions. However,
the 2015 National Academy of Medicine report established ME/CFS as a positive diagnosis that can coexist with other conditions, including those in the differential diagnosis. Recognizing co-morbid conditions early and treating them appropriately may improve the patient’s health, function, and quality of life. Commonly comorbid conditions include:TREATING AND MANAGING ME/CFS (THE BASICS)
In the past, ME/CFS has been characterized as a syndrome of medically unexplained fatigue responsive to talk therapy and graded exercise. But scientific advances are revealing a complex, multisystem disease involving neurological, immunological, autonomic, and energy metabolism impairments. There is a critical need for a different approach to management of the disease and accompanying comorbidities.1. Validate the patient experience and educate about the disease
Patients may have experienced skepticism about their disease. The most important thing that a medical provider can do is to validate the illness for the patient and the patient’s family. Explain that ME/CFS is a serious medical illness and is not laziness, depression, or a psychosomatic disorder.2. Address impaired function and provide support as needed
By definition, patients with ME/CFS have significant disability. Patients may need help in obtaining accommodations for school and work or when applying for disability. They may also need parking permits, assistive devices, and/or home health aides. Because of the financial impact, some patients may need help with shelter and food. Many may also lose their health insurance.3. Educate patients about pacing to prevent or minimize PEM
An important role for the medical provider is to teach patients about PEM and how to manage it with pacing. Pacing is an individualized approach to managing physical, cognitive, and emotional energy within a patient’s specific limits by carefully planning where and how to spend their available energy.
It is a critical tool to prevent and/or reduce PEM. Activity logs and heart rate and activity monitors can be used to help patients understand when they are overdoing their specific energy limits. Even with such aids, pacing is a challenging task and some setbacks are inevitable, especially since tolerance for
activity can vary from patient to patient and day to day.4. Treat/manage symptoms (*)
While there are no treatments approved specifically for ME/CFS, a number of different pharmacological and non-pharmacological treatments can help reduce the severity of symptoms. Some examples of commonly used medications include low-dose naltrexone, duloxetine, gabapentin, or
pregabalin for pain; fludrocortisone, midodrine, pyridostigmine, low dose beta-blockers and/or
intravenous hydration for orthostatic intolerance; occasional use of modafinil, methylphenidate, or dexedrine for cognitive or fatigue issues; and trazodone, clonazepam, tricyclic antidepressants, or suvorexant for sleep. Drugs should be started at low doses and increased slowly to avoid triggering
drug sensitivities common in ME/CFS.Non-pharmacological approaches include: salt and fluid loading and compression stockings for those with orthostatic problems; cognitive aids (e.g. writing notes to assist memory; keeping a calendar, notebook and calculator at hand; and always placing important items in the same place); ear plugs, eye masks and sunglasses for those with light and sound sensitivities; sleep hygiene measures; and avoidance of problematic foods and meditation.
Note: In addition to these basic treatments, some disease experts are evaluating the selective use of antivirals and immune modulators in ME/CFS and have seen evidence of efficacy in some patients.
(*) This is not an exhaustive list of treatments. For further information on these and other treatments,
see the references for the Adult and Pediatric Primers below.5. Treat Comorbid Conditions
As listed earlier, a number of conditions may be comorbid with ME/CFS. Treating these comorbid conditions using the appropriate standard of care will not cure ME/CFS but it may improve the patient’s quality of life.BASIC FACTS
▪ ME/CFS affects an estimated 836,000 to 2.5 million Americans but an estimated 84 to 91 percent of
patients have not yet been diagnosed.
▪ ME/CFS affects 3 times as many women as men.
▪ Most patients currently diagnosed with ME/CFS are Caucasian, but some studies suggest ME/CFS is
more common in minority groups.
▪ ME/CFS has been reported in patients younger than age 10 and older than age 70. Studies have shown
one peak of onset between 11-19 and a second between 30-39.
▪ At least 25% of patients are bedbound or housebound and up to 75% are unable to work or attend
school.
▪ Symptoms can persist for years, and most patients never regain their pre-disease functioning.
▪ ME/CFS costs the US $17 to $24 billion annually in lost productivity and direct medical costs.
▪ The cause of ME/CFS is unknown, although the disease often follows an infection.USEFUL REFERENCES
▪ US ME/CFS Clinician Coalition Website https://mecfscliniciancoalition.org/
▪ US ME/CFS Clinician Coalition Testing Recommendations
http://mecfscliniciancoalition.org//MECFS-Clinician-Coalition-Testing-Recs-V1
▪ US ME/CFS Clinician Coalition Treatment Recommendations
http://mecfscliniciancoalition.org//MECFS-Clinician-Coalition-Treatment-Recs-V1
▪ Beyond Myalgic Encephalomyelitis/Chronic Fatigue Syndrome: Redefining an Illness. National Academy of
Medicine, formerly called the Institute of Medicine. 2015. Includes report and Clinician Guide.
http://www.nationalacademies.org/hmd/Reports/2015/ME-CFS.aspx
▪ Komaroff, Anthony L. “Advances in Understanding the Pathophysiology of Chronic Fatigue
Syndrome.” JAMA 322, no. 6 (August 13, 2019): 499. https://doi.org/10.1001/jama.2019.8312
▪ Myalgic Encephalomyelitis/Chronic Fatigue Syndrome: Clinical Working Case Definition, Diagnostic and
Treatment Protocols. (Canadian Consensus Criteria), 2003. Provides expanded criteria
https://phoenixrising.me/wp-content/uploads/Canadian-definition.pdf
▪ Myalgic Encephalomyelitis: International Consensus Criteria. (ME-ICC criteria). 2011. Provides expanded
criteria. https://onlinelibrary.wiley.com/doi/full/10.1111/j.1365-2796.2011.02428.x
▪ Chronic Fatigue syndrome/Myalgic Encephalomyelitis. Primer for Clinical Practitioners.
2014 Edition. International Association for Chronic Fatigue syndrome/Myalgic Encephalomyelitis
https://www.iacfsme.org/assets/docs/Primer_Post_2014_conference.pdf (Activity log in Appendix D)
▪ Rowe, P et al. Myalgic Encephalomyelitis/Chronic Fatigue Syndrome Diagnosis and Management in Young
People: A Primer. Frontiers in Pediatrics. June 2017. Pages 8-12 provides information on differential diagnosis,
including for psychiatric illness https://www.frontiersin.org/articles/10.3389/fped.2017.00121/full
▪ CDC ME/CFS Website: Information for HealthCare Providers
https://www.cdc.gov/me-cfs/healthcare-providers/index.html
▪ Rowe, P. General Information Brochure On Orthostatic Intolerance And Its Treatment.
March 2014. https://www.dysautonomiainternational.org/pdf/RoweOIsummary.pdf
▪ Bateman Horne Center. NASA 10 Minute Lean Test – Instructions for Providers.
http://batemanhornecenter.org/wp-content/uploads/2016/09/NASA-LeanTest-Instructions-April-2018.pdf
▪ Campbell B, Lapp C. Treating Chronic Fatigue Syndrome and Fibromyalgia. Pacing Guidance.
http://www.treatcfsfm.org/menu-Pacing-7.html