[8-4-2018 This post is now out of date please see my new post with links to the new versions of the documents listed below: Improving Access to Psychological Therapy (IAPT) – Help For Primary Care Physicians From The National Health Service Posted on August 4, 2018.]
Improving Access to Psychological Therapy (IAPT) from the National Health Service (NHS)
Improving Access to Psychological Therapy
The IAPT Data Handbook: Guidance on recording and monitoring outcomes to support local evidence-based practice. 2011.
See also the link to the IAPT Data Handbook Appendices.
See also
Talking therapies:
A four-year plan of action 2011
All of that follows is from the IAPT Data Handbook:
p 18
Arriving at a provisional diagnosis
The IAPT Data Standard provides a coding framework for the range of diagnoses suitable for treatment within IAPT services, including relevant ICD-10 coding. On determination of an anxiety disorder provisional diagnosis by the IAPT worker at initial assessment, the appropriate outcome measurement tools can be applied from the range of relevant anxiety disorder specific measures (ADSMs). The ADSMs are further outlined below and presented in detail at Appendix D.
Following guidance from professional bodies, the term “Diagnosis” will henceforth be more accurately referred to as ‘Provisional Diagnosis’. Provisional diagnoses record patterns of symptoms and do not replace in any way the patient-centred assessment required to personalize treatment plans.
Provisional diagnoses are needed as specific treatments have been developed to assist people with particular symptom patterns and NICE guidelines are diagnosis based. We can therefore only ensure that patients receive the best treatments in line with NICE recommendations if provisional diagnoses have been obtained. Provisional diagnosis should not be viewed as a pejorative label. Many patients feel diagnosis is useful to reassure them that there are others with similar patterns and difficulties.
p 19
Appendix C provides a series of screening questions to support clinicians arriving at provisional diagnoses, aligned to ICD-10 codes (see WHO 1994 https://apps.who.int/classifications/apps/icd/icd10online/ questions and prompts listed are intended to address key differentiating symptoms that will aid IAPT workers in coming to a provisional diagnosis.
The screening questions at Appendix C are not, of course, a substitute for thorough clinical
judgment – where there is serious concern or doubt a specialist opinion should be sought. A risk assessment and/or review should always be undertaken as part of all clinical contacts. Clinical leads are appointed for each IAPT service region and are responsible for ensuring that clinical governance procedures, such as for assessing and managing risk to self and others, are followed by all IAPT workers involved in patient assessments.
There are certain people with primary diagnoses that the IAPT service would not ordinarily treat directly (e.g. people with eating disorders or psychosis). However, IAPT services exist within a wider landscape of mental health service provision and services need to determine care pathways for these patients, including referral to other services that may be more appropriate to meet their needs. This will entail links with specialist health clinics and secondary care health sectors, working collaboratively to improve the health outcomes of individual patients.
Measuring clinical, work and social functioning outcomes
The IAPT outcome measures are:
• Patient Health Questionnaire (PHQ-9) for depression
• Generalised Anxiety Disorder Assessment (GAD7)
• IAPT phobia scales
• Work and Social Adjustment Scale (WSAS)
• IAPT employment status questions
• A range of relevant anxiety disorder specific measures (ADSMs)
• IAPT patient choice and experience questionnaire
p 20
All measures are included in appendices D and E. These measures are the most suitable, free to access and widely used tools available. Copyright holders have granted permission to the IAPT programme for these measures to form part of the IAPT Data Standard. Permission has been obtained by NHS Connecting for Health (CfH) for the inclusion of these outcome measures, on NHS electronic patient management systems where they can be included in full.
Measures should be taken near the beginning of most clinical contacts. They can often be
completed whilst patients are waiting for appointments or earlier on the day of the appointment. On some occasions, the IAPT worker may wish patients to complete measures within sessions in order to introduce them to the measures and to engage them in the process of objective measurement of symptoms. At first contact, IAPT workers may wish to engage patients through a patient/problem focussed interview before moving onto the collection of measures, as detailed in the example low-intensity interview schedules (contained within the IAPT ‘Reach Out’ low intensity curriculum support materials – https://www.iapt.nhs.uk/silo/files/reach-out-educatormanual.pdf).
However, some patients will have already been asked to complete the PHQ-9 by
their GP or other clinician to identify whether they should be referred to an IAPT service.
Measures such as the PHQ-9 and GAD7 do not replace comprehensive clinical interview
assessments of need and should not be used as the sole basis on which to include or exclude patients from services. When undertaking remote sessions, such as via telephone or email, IAPT workers should ensure that patients have copies of the required IAPT clinical outcomes measures to complete so that scores can be collected quickly and efficiently. The IAPT worker should always carefully explain the rationale for using measures and should feedback their scores routinely to monitor progress and confirm patient narrative accounts of their progress.
Sharing outcome scores with patients
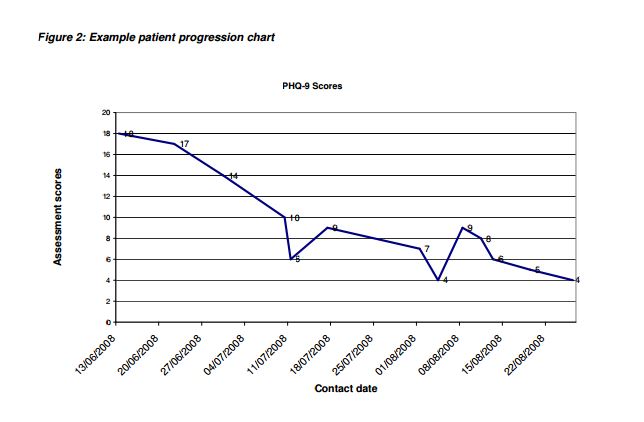
In putting patients at the centre of the IAPT care pathway, it is important that each person using the service sees their scores from their completed questionnaires, and sees how their scores change over time. The scores help patients to understand more about their condition and can help establish and develop the therapeutic relationship. GPs and early IAPT sites found this approach to be positively therapeutic. Similarly, seeing how patient outcome scores change over time, both for those who are improving and for those not responding to treatment, is also helpful to clinicians. Figure 2 depicts a patient progression chart. Clinicians may need to consider, with the patient, alternative interventions including step-ups from low to high-intensity
treatment.
Data that can be useful to report to the patient include:
• Individual scores
• Sequential outcome scores over time
• The recovery pattern (changing outcome scores over time) expressed as an average
score over time.
p 21
Clinical leads and service managers should ensure all IAPT workers have access to up to date reports and charts showing the patient’s progress through the care pathway. It is essential that patients and IAPT workers have access to clinical progress data at each patient session. Supervisors will also need access to the same real-time data to ensure effective supervision and timely intervention where necessary (see Chapter 3). In addition, IAPT workers can benefit from aggregated outcome scores for everyone that they have treated as a means to understanding the effectiveness of the interventions they are delivering, with the support of their supervisor. Reports are covered in more detail in Chapter 3.
p 22
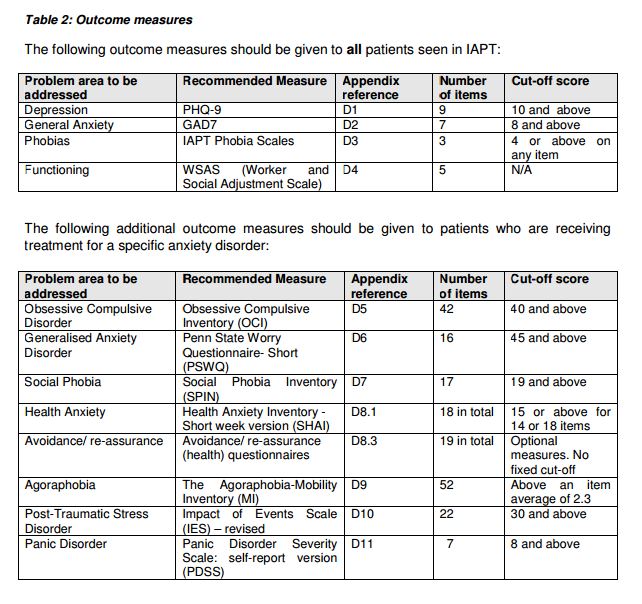
IAPT Clinical Outcome Measures
All IAPT outcome measures are summarised in Table 2, including details on cut off scores for clinical caseness, scores above which correlate with diagnosis of a disorder.
Depression – PHQ-9
The nine item version of the Patient Health Questionnaire (PHQ-9) was designed to facilitate the recognition and diagnosis of depression in primary care patients. It can be used to monitor change in symptoms over time and provides a depression severity index score as follows:
0 – 4 None
5 – 9 Mild
10 – 14 Moderate
15 – 19 Moderately Severe
20 – 27 Severe
The recommended cut-off for the PHQ-9 severity index is a score of 9. Anyone who scores 10 or above can be considered to be suffering from clinically significant symptoms of depression. This is referred to as meeting “caseness”.
Generalised Anxiety Disorder – GAD7
Though designed primarily as a screening and severity measure for generalised anxiety
disorder, the GAD7 also has moderately good operating characteristics for three other common
anxiety disorders – panic disorder, social anxiety disorder, and post-traumatic stress disorder.
The index scores are as follows:
0 – 4 None
5 – 10 Mild Anxiety
11 – 15 Moderate Anxiety
15 – 21 Severe anxiety
The recommended cut off for the GAD7 severity index is a score of 7. Anyone who scores or above can be considered to be suffering from clinically significant anxiety symptoms.
IAPT Phobia Questions
These questions are included because it is clear that some patients (such as people with
agoraphobia and social phobia) score below the clinical cut-offs for the PHQ-9 and GAD7 even
though their life is significantly impaired by their anxiety disorder. This is because marked
avoidance (such as being housebound) means that they may not experience strong anxious
affect on a daily basis. PHQ-9/GAD7 would not measure clinical improvement in such
individuals.
Currently the three IAPT phobia questions have not been validated as screening instruments.
The questions that are included in the IAPT Data Standard are based on the approach to
measurement of the severity of phobias used in the Marks & Matthews Fear Questionnaire and many other similar fear questionnaires. Many clinical trials of treatments for phobias exclude patients if they score less than 4 on a 0-8 phobia scale at pre-treatment. If the patient scores 4 or above on any of the three phobia questions at intake, assessors should enquire about the extent to which a phobia is present and interfering with a patient’s life. Appendix C provides a series of screening questions to support clinicians arriving at provisional diagnoses where phobia may form a significant component and the application of particular ADSM may be relevant. The decision to treat will be a mutual one based on the outcome of that enquiry. Furthermore, the appropriate anxiety disorder specific measure should be used to assess and to monitor clinical improvement.
p 24
Work and Social Adjustment Scale (WSAS)
The Work and Social Adjustment Scale (WSAS) is a simple 5-item patient self-report measure, which assesses the impact of a person’s mental health difficulties on their ability to function in terms of work, home management, social leisure, private leisure and personal or family relationships. The WSAS is used for all patients with depression or anxiety as well as phobic disorders.
Employment and Benefit Status
Questions relating to employment, benefits status and sick pay should be asked on a sessional basis and should be recorded on systems.
The IAPT worker records the patient’s status with regard to employment, and whether they arein receipt of sick pay. Then, on a sessional basis, changes in this status can be recorded. Receipt of sick pay from an employer should be recorded as receipt of Statutory Sick Pay (SSP) as it is assumed that the employer will claim SSP in respect of their employee’s absence.
The employment status data item in the IAPT Data Standard includes reference to a range of other benefits. This data item is a standard NHS data dictionary item and the value of these categories for IAPT services will be evaluated through future review and consultation. Referral to employment support services should also be recorded. A need for employment support is indicated where the individual is:
• Regularly absent from work
• On statutory or employer sick pay (and therefore at risk of moving on to ill-health
related benefits)
• On ill-health related benefits
• Citing difficulties at work
Where employment services are provided in IAPT, service managers should consider implementing extended data sets that capture a broader range of measures. The impact of aco-ordinated IAPT employment service on patient health outcomes, and evidence of aneffective service model, is indicated by measures derived from enhanced data sets.
p 25
IAPT Recommended Anxiety Disorder Specific Measures (ADSM)
It is common for people with several different disorders to score highly on both the PHQ-9 and GAD7 (e.g. Depression, Social Phobia, PTSD, OCD). However, the treatments for these disorders are significantly different and therefore making a differential provisional diagnosis is crucial to ensure that appropriate clinical care is provided. This should be part of a full personcentredassessment (see above, and Appendix C for advice in arriving at a provisional diagnosis).
The recommended IAPT anxiety disorder specific measures (ADSM) should be used whenever a relevant condition is being treated, in addition to other IAPT outcome measures. The anxiety disorder measures are not only used to confirm identification and severity of the disorder. They should also be used to monitor patient progress and recovery using the cut-off for caseness shown in Table 2, and described in further detail below.
Most of the ADSMs (PSWQ, SPIN, SHAI, IES-revised, PDSS) are suitable for administration every session. Some (the OCI and MI) are more suitable for administration every few sessions but should still be given repeatedly during the course of therapy in order to ensure that a posttreatment score is available even in patients who drop out of treatment.
p 26
Case Study: Measuring recovery using an ADSM:
John presented for treatment because he was feeling low and irritable, had
problems sleeping and concentrating, and felt unable to work. At assessment, he
mentioned the problems started two years ago after he had been assaulted. The
Impact of Events Scale (IES-R) confirmed the severity of John’s symptoms of
PTSD, and the therapist started a course of trauma-focused CBT for PTSD.
Session by session administration of the IES-R showed that imaginal reliving of
the trauma memory in therapy had only a modest effect on John’s re-experiencing
symptoms (flashbacks, intrusive images). Discussion of the IES-R scores revealed
that the re-experiencing symptoms related to moments in the trauma that John
had not mentioned to the therapist. When these moments were addressed in
treatment, John’s symptoms declined and he slept much better. However, he was
still having trouble concentrating and felt irritable. An IES-R item showed that
John felt “watchful and on guard”. Treatment then focused on his belief that he
could not trust other people after the trauma. As a consequence, his
concentration and irritability improved.
Each of the recommended Anxiety Disorder Specific Measures are considered in detail below, and further information may be available in the References section of this Handbook.
Obsessive Compulsive Disorder
The Obsessive Compulsive Inventory (OCI) has 42 Items and a cut-off score of 40 and above. It is recommended where the provisional diagnosis is Obsessive Compulsive Disorder.
This measure provides an obsessive compulsive disorder severity score from ratings of the extent to which particular experiences have distressed or bothered the patient in the last month.
Scoring: 0-4 Item Scale; 0=Not at all; 4=Extremely
Generalised Anxiety Disorder
The Penn State Worry Questionnaire (PSWQ) has 16 items and a cut-off score of 45 and
above. It is recommended where the provisional diagnosis is Generalized Anxiety Disorder.
This measure provides a generalised anxiety disorder severity score based on ratings indicating how typical or characteristic particular statements are.
Scoring: 1-5 Item Scale; 1=Not at all typical; 5=Very typical.
A final score is derived from the total of all scores after reversing specific items as follows then summing all 16 items;
Reverse score items; 1, 3, 8, 10 and 11,
Very typical of me = 1 (circled 4 on the sheet);
Circled 3 on the sheet =2;
Circled 2 on the sheet = 3;
Circled 1 on the sheet = 4;
Not at all typical of me = 5 (circled 1 on the sheet).
p 27
Social Phobia
The Social Phobia Inventory (SPIN) has 17 items and a cut-off score of 19 or above. It is
recommended where the provisional diagnosis is Social Phobia.
For each item, patients select a number to indicate how bothered they have been by the item during the past week. The total score provides a measure of the severity of social phobia.
Scoring: 0-4 Scale for each item; 0 Not at all; 4 Extremely
Health Anxiety
The Health Anxiety Inventory (Short version; SHAI) has 14 items in the main section and 4 in another section. The main section should be used sessionally with those patients who have health anxiety. A cut-off score of 15 indicates a mixture of both hypochondriacal patients and people who are very health anxious but just miss the criteria for the clinical diagnosis; a cut-off of 18 or higher identifies people fulfilling DSM-IV diagnostic criteria for hypochondriasis.
At an initial assessment, mid-treatment and end of treatment it is appropriate to use all 18 items. At the initial treatment or for general screening it is appropriate to ask the patient about their feelings in the preceding 6 month period, consistent with the diagnostic criteria for Hypochondriasis. When monitoring treatment response at other times, i.e. sessionally, applying the 14 main scale questions is recommended for the sake of brevity.
Scoring: a)-d) Item Scale; a) scores 0, d) scores 3.
p 28
Agoraphobia
The Agoraphobia-Mobility Inventory (MI) has 27 items. It is recommended where the
provisional diagnosis is Agoraphobia.
Patients select numbers to indicate the degree to which they would avoid particular places or
situations because of discomfort or anxiety. The total score provides a measure of the severity
of agoraphobia.
Scoring: 1-5 item scale: 1 Never avoid, 2 Rarely avoid, 3 Avoid about half the time, 4 Avoid
most of the time, 5 Always avoid.
Each situation is rated twice to reflect the degree that the situation is avoided by the
agoraphobic participant when he or she is alone, and when he or she is accompanied.
Participants may skip items that are irrelevant to their lifestyles; however, Chambless et al.
(1985) recommend that the scale be considered invalid for individuals who skip more than five items (20%). The MI is scored by calculating the average avoidance rating across all situations for the ‘When alone’ and ‘When accompanied’ scales. For the measure related to ‘When alone’ a cut-off score above an item average of 2.3 should be applied.
Post Traumatic Stress Disorder
The Impact of Events Scale Revised (IES-R) has 22 items and a cut-off score of 30 or above. It
is recommended where the provisional diagnosis is Post Traumatic Stress Disorder (PTSD).
Patients select numbers to indicate how frequently particular comments have been true during
the past seven days. The total score provides a measure of the severity of PTSD.
Scoring: 0-4 Item; 0 Not at all, 4 Extremely.
The total score is derived from the sum of three clinical scales;
Avoidance Subscale: Mean of items 5, 7, 8, 11, 12, 13, 17, 22.
Intrusions Subscale: Mean of items 1, 2, 3, 6, 9, 16, 20.
Hyperarousal Subscale: Mean of items 4, 10, 14, 15, 18, 19, 21.
p 29
Panic Disorder
The Panic Disorder Severity Scale (PDSS) has 7 items and a cut-off score of 8.
The PDSS is a simple, reliable instrument for use in Panic Disorder studies. A cut-score of 8 may be useful as a tool to screen patients in settings such as primary care, for diagnosis-level symptoms (Shear, M. K., P. Rucci, et al. (2001)).
For scoring advice see: https://goodmedicine.org.uk/files/panic,%20assessment%20pdss,%20scoring.doc
p 43
IAPT Recommended Outcome Measures
Additional Resources:
(1) The IAPT Data Handbook Appendices: Including the IAPT Data Standard. June 2011.
Contents
A. IAPT Data Standard (v1.6)
B. NICE-indicated Treatments for Depression and Anxiety
C. IAPT Provisional Diagnosis Screening Prompts
D. IAPT Measurement tools
E. IAPT Information System Commissioning Guidance
F. IAPT Key Performance Indicator Technical Guidance
G. IAPT Information Governance
H. Patient Information Leaflet
(2) Extracts From and A Link To COMMON MENTAL HEALTH DISORDERS: THE NICE GUIDELINE ON IDENTIFICATION AND PATHWAYS TO CARE, 2011. Posted on January 23, 2015 by Tom Wade MD
(3) Reach Out: National Programme Educator Materials to Support the Delivery of Training for Psychological Wellbeing Practitioners Delivering Low Intensity Interventions. David Richards and Mark Whyte, 2nd edition, 2009.