In addition to today’s resource from Emergency Medicine Cases, please see
Reversible Cerebral Vasoconstriction Syndromes
Omar Nesheiwat; Lama Al-Khoury.Author Information and
Last Update: July 4, 2022. From StatPearls.
Primary Central Nervous System Vasculitis
Raja Godasi; Graeme Pang; Shaylika Chauhan; Pradeep C. Bollu. Last Update: October 12, 2022. From StatPearls.
Posterior Reversible Encephalopathy Syndrome
Jaime E. Zelaya; Lama Al-Khoury.Last Update: May 1, 2022. From StatPearls.
In this post, I link to and excerpt from Emergency Medicine Cases‘ podcast, Ep 161 Red Flag Headaches: General Approach and Cervical Artery Dissections*.
* Helman, A. Shah, A. Baskind, B. Episode 161 Red Flag Headaches: General Approach and Cervical Artery Dissections. Emergency Medicine Cases. November, 2021. https://emergencymedicinecases.com/red-flag-headaches-cervical-artery-dissections. Accessed 5-22-2023.
All that follows is from the outstanding show notes.
The big 4 causes of emergency headaches that are not routinely identified on plain CT
Headaches are one the most common ED presentations. About 98% of these patients have a benign cause of their headache. Of the remaining 2%, 1% can be diagnosed with a CT head or LP, such as a subarachnoid hemorrhage or meningitis, however the final 1% causes of headaches cannot be ruled out on plain CT/LP alone. The big four commonly missed emergency causes of headaches that cannot routinely be ruled out on plain CT:
- Cervical artery dissection (carotid and vertebral)
- Cerebral venous thrombosis (CVT)
- CO poisoning
- Giant cell arteritis
In this part 1 of our 2-part podcast on red flag headaches we focus on a general approach to headaches in the ED and cervical artery dissection – one of the big five causes of emergency headaches that does not show up routinely on plain CT, requiring a CT angiogram of the head and neck to confirm the diagnosis.
Some clinical pearls for headache assessment
- Headaches can arise from referred pain from the neck and neck pain can arise from referred pain from the head; include neck pathology in patients who present with headache and vice versa
- Clinical features that should trigger the consideration for a serious cause of headache include rapid onset of pain within minutes, repeat visits to ED for the same headache, exertional headache, different to previous headaches, focal neurologic findings, papilledema, immunocompromised state, loss of vision and abnormal vital signs
Dr. Baskind’s general approach to headache differential diagnosis: MY BRAIN HURTS
*Reversible Cerebral Vasoconstriction Syndromes
Omar Nesheiwat; Lama Al-Khoury.Author Information and
Last Update: July 4, 2022. From StatPearls.*Primary Central Nervous System Vasculitis
Raja Godasi; Graeme Pang; Shaylika Chauhan; Pradeep C. Bollu. Last Update: October 12, 2022. From StatPearls.*Posterior Reversible Encephalopathy Syndrome
Jaime E. Zelaya; Lama Al-Khoury.Last Update: May 1, 2022. From StatPearls.
Update 2021: Tertiary pediatric center study of using rapid sequence brain magnetic resonance imaging (RS-MRI) as a feasible screening tool in 105 children (<12 years old) with persistent/recurrent headaches. 77% out of 105 cases were normal, 23% were abnormal; notably, 75% diagnosed with sinusitis, and 1 case with an abnormal brain mass. Abstract 
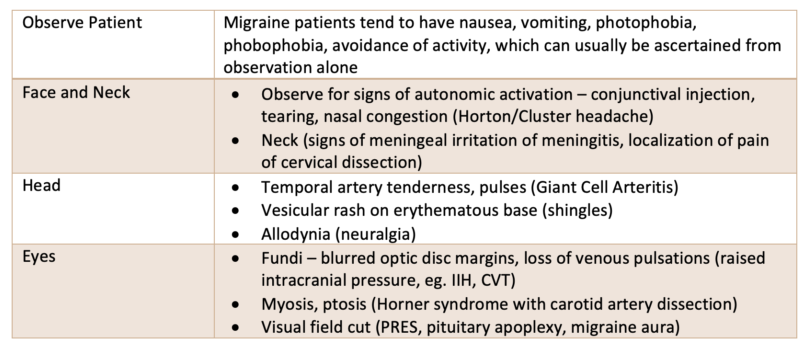
Dr. Baskind’s physical examination tips suggesting specific diagnoses for patients presenting with headache
Cervical artery dissection is often difficult to diagnose in the ED
Carotid and vertebral artery dissections cause up to 25% of strokes in young patients. They can occur spontaneously or following neck trauma, which may be minor in force. They are difficult to diagnose, especially on initial visit to the ED, because headache and/or neck pain may be their only symptom(s), stroke symptoms, which occur in a about 2/3 of patients, may be delayed by hours, days or even weeks, and neurologic deficits may be fluctuating, transient (may be completely resolved by the time they present to the ED), and often do not fit a typical stroke large vessel arterial distribution.
Pathophysiology of cervical artery dissection is important to help understand the clinical features
A tear occurs in the intimal lining of the artery which initiates a dissection along the length of the artery. This typically coincides with the acute head/face/neck pain that may be migratory. An intramural hematoma develops with subintimal dissections that lead to stenosis and may also cause complete occlusion. Thrombi may dislodge causing downstream occlusion and showering of emboli can flow to various locations causing a variety of neurologic symptoms that do not fit a typical large vessel occlusion distribution. In addition to the ischemic phenomena there may be concurrent stretching of vessel by the local clot/distension which can have local peripheral neurologic effects such as partial Horner’s Syndrome and cranial neuropathies.
Key take home points for red flag headaches general approach and cervical artery dissections
- The big five commonly missed emergency causes of headaches that cannot routinely be ruled out on plain CT/LP include: Cervical artery dissection, CVT, Idiopathic Intracranial Hypertension, CO poisoning, Giant cell arteritis
- Spinal pathology may present with headache and CNS pathology may present with neck pain – include neck pathology in patient who present with headache and vice versa
- Use MY BRAIN HURTS mnemonic to run through the differential diagnosis of patients who present to the ED with headache
- Up to 25% of strokes in young patients are caused by cervical artery dissections – young people get strokes!
- Cervical artery dissections can present with pain only without any other symptoms, and may be spontaneous or traumatic
- Delayed, fluctuating and transient seemingly “non-anatomical” neurologic symptoms that range from vertigo to amaurosis fugax to large vessel stroke syndromes are not uncommon in patients with cervical artery dissection; their neurologic exam may be completely normal in the ED
- Migraines cause ipsilateral neurological symptoms; carotid artery dissections cause contralateral symptoms whereas vertebral artery dissections can cause contralateral or bilateral symptoms
- Examine carefully for partial partial Horner’s Syndrome which is found in some patients with carotid artery dissection
- LMWH is the most commonly used antithrombotic treatment used in extracranial cervical artery dissections, but the evidence is not clear for clinical benefit compared to ASA
- Patients with stable pain and normal neurologic exam can be considered for safe discharge from the ED
- If in doubt after plain CT and no contraindications, if there is a delay to CT angiogram, it is reasonable give the patient ASA in the ED and a script for ASA until they see neurologist in follow-up, although there is no good evidence supporting this practice
Learn more about cervical artery dissection at Episode 14 Part 2: Thunderclap Headache- Cerebral Venous Thrombosis and Cervical Artery Dissection