Accurate determination of the respiratory rate is critical in pediatrics. A respiratory rate of greater than 60 in the neonate or infant is almost always abnormal and at the least needs to be evaluated and explained.
A respiratory rate of greater than 40 is abnormal in patients aged 1 year to 5 years of age and also needs to be evaluated and explained.
See Common causes of Tachypnea in children.
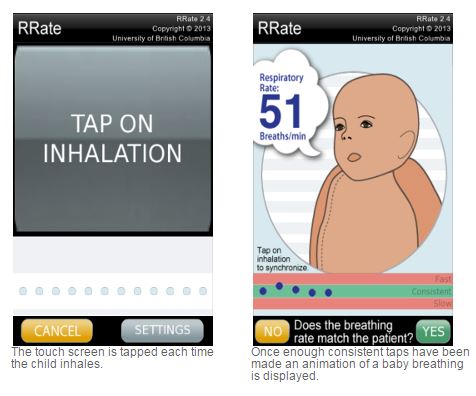
The authors developed “a mobile phone application that calculates the RR by measuring the time intervals between breaths by tapping the screen of a mobile device. Efficiency E was significantly improved compared to conventional methods that require
counting for 60 s.”
The authors developed the “RRate mobile application, which is freely available for download [14,15].”
The RRate mobile app is available for download at Google Play and Itunes. To learn more about the app visit the app’s website.
The following is from Reference (1), Improving the accuracy and efficiency of respiratory rate measurements in children using mobile devices June 2014:
Introduction
Respiratory rate (RR) plays a fundamental role in routine
clinical assessment for disease diagnosis, prognosis, and treatment in children [1]. Accurate measurement of RR is of paramountimportance because an elevated RR is a marker of serious respiratory illness [2] and is the main diagnostic criterion forchildhood pneumonia [1], the leading cause of death in childrenaged 0 to 5 years worldwide [3]. However, many studies have demonstrated clinically obtained measures to be inaccurate,lacking both reliability and reproducibility in a variety of health care settings [4–6].
The current recommended method for measuring RR is to
count the number of breaths in one minute. This method was
promoted by the World Health Organization (WHO) [7], and
since 1990 facilitated by the distribution of the Acute Respiratory Infection (ARI) Timer in the developing world. The ARI Timer is a simple device providing auditory feedback in the form of ticks at 1 s intervals for 60 s. The ARI Timer has shown many limitations in the field, mostly related to usability aspects [8,9]. The measurement duration of 60 s is perceived to be too time consuming. Also, counting the number of breaths in a fixed
amount of time requires that measurements be restarted from the beginning in case of a noticed artifact (e.g. missing a breath) or distraction, further increasing total measurement time. Counting the number of breaths over 60 s can be especially difficult in sick children who may breathe at a rate that is upwards of 60–70 breaths/min. In practice, health care workers do not count RR for a whole minute, but instead count for only a fraction of 60 s and then scale up the number of breaths to 60 s. This decreases the accuracy of RR measurement by amplifying the counting error [10]. Thus, there is an urgent need for a robust, low-cost device that can help front-line health care workers to measure RR quickly and accurately. An effective way for improving efficiency and accuracy of rate estimations is incremental and continuous analysis of time intervals instead of counting events in a fixed time interval [11]. However, there is a trade-off between accuracy and efficiency which has to be addressed by design [10].Discussion
We developed a mobile phone application that calculates the
RR by measuring the time intervals between breaths by tapping
the screen of a mobile device. Efficiency E was significantly
improved compared to conventional methods that require
counting for 60 s. The introduction of a consistency threshold
ThC eliminated inconsistent user input and reduced the NRMSE
significantly. The mobile phone application RRate required the user to tap on a touch sensitive screen in time with inhalation, and the tap interval times were recorded into a set. The median of a set of tap intervals was calculated and each interval was checked for consistency. If all intervals were within a consistency range, the RR was reported as 60 s divided by the median. With our experiments, we have demonstrated that the median efficiency ~EE improved from 60 s to a mean of 8.161.2 s and a mean 95th percentile of 17.662.7 s. This was a significant reduction of time required for achieving a reasonable estimation of RR. The mean NRMSE of 5.6% corresponded to an error of 2.2 breaths/min at the critical RR of 40 breaths/min which is the diagnostic threshold for fast breathing in children aged 1 to 5 years [1].Mobile technology is ubiquitous, even in developing countries
and rural parts of the world [12]. A growing number of initiatives
are using mobile phones to tackle the health challenges of
developing countries [12]. One of these challenges is the accurate
measurement of RR in children. We proposed a RR estimation
algorithm based on measuring the time intervals between breaths
that allows a 6-fold increase in mean efficiency compared to the
current recommended method of counting breaths for 60 s with
the ARI Timer. This algorithm was implemented into the RRate
mobile application, which is freely available for download [14,15].
With the reduction in cost and widespread use of smart phones
and mobile devices, such mobile applications may be a promising replacement for the ARI Timer. Vibro-tactile and visual feedback allows the user to focus on the patient and to obtain feedback for
quality assurance at completion of measurement. We are currently undertaking a direct comparison between the RRate and the ARI Timer for accuracy, efficiency and usability. Further validation including clinical testing in the target environment with community health workers assessing sick children will be necessary to demonstrate positive impact on diagnosis of pneumonia and other respiratory diseases with the RRate application.
Resources:
(1) Improving the accuracy and efficiency of respiratory rate measurements in children using mobile devices [PubMed Abstract] [Full Text HTML] [Full Text PDF]. PLoS One. 2014 Jun 11;9(6):e99266. doi: 10.1371/journal.pone.0099266. eCollection 2014.
(2) Correction: Improving the accuracy and efficiency of respiratory rate measurements in children using mobile devices [PubMed Abstract] [Full Text HTML] [Full Text PDF]. PLoS One. 2015 Feb 6;10(2):e0118260. doi: 10.1371/journal.pone.0118260. eCollection 2015.
(3)