I’ve divided these posts, my study notes on the European high blood pressure guidelines, into several parts for ease of my review. Links to all my post on the 2018 European Hypertension Guidelines are in Additional Resources after this post.
The following are excerpts from the Resistant Hypertension section from the 2018 ESC/ESH Guidelines for the management of arterial hypertension [PubMed Abstract] [Full Text HTML] [Full Text PDF]. Eur Heart J. 2018 Sep 1;39(33):3021-3104. doi: 10.1093/eurheartj/ehy339:
8.1 Resistant hypertension
8.1.1 Definition of resistant hypertension
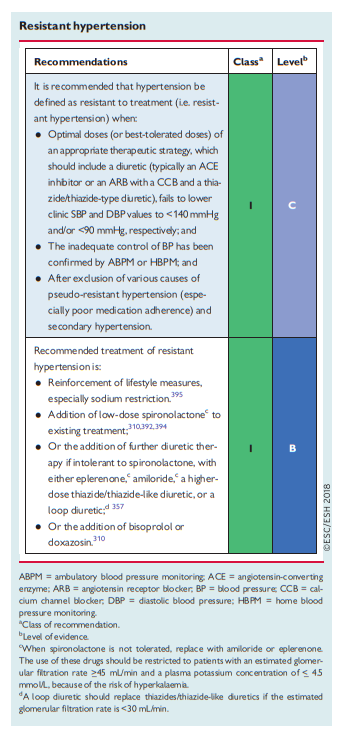
Hypertension is defined as resistant to treatment when the recommended treatment strategy fails to lower office SBP and DBP values to <140 mmHg and/or <90 mmHg, respectively, and the inadequate control of BP is confirmed by ABPM or HBPM in patients whose adherence to therapy has been confirmed. The recommended treatment strategy should include appropriate lifestyle measures and treatment with optimal or best-tolerated doses of three or more drugs, which should include a diuretic, typically an ACE inhibitor or an ARB, and a CCB. Pseudo-resistant hypertension (see below) and
secondary causes of hypertension should also have been excluded (see section 8.2).Prevalence studies of resistant hypertension have been limited by variation in the definition used, and reported prevalence rates range from 5–30% in patients with treated hypertension. After applying a strict definition (see above) and having excluded causes of pseudoresistant hypertension (see section 8.1.2), the true prevalence of resistant hypertension is likely to be <10% of treated patients. Patients with resistant hypertension are at higher risk of HMOD, CKD, and premature CV events.382
8.1.2 Pseudo-resistant hypertension
Several possible causes of pseudo-resistant hypertension should be evaluated and ruled out before concluding that the patient has resistant hypertension:
(1) Poor adherence to prescribed medicines is a frequent cause
of pseudo-resistant hypertension, occurring in <_50% of patients assessed by therapeutic drug monitoring, and is directly related to the number of tablets prescribed315 (see section 10).(2) White-coat phenomenon (in which office BP is elevated but BP is controlled at ABPM or HBPM) is not uncommon in these
patients, hence the recommendation to confirm office hypertension with ABPM or HBPM before confirming the diagnosis of resistant hypertension.(3) Poor office BP measurement technique, including the use of
cuffs that are too small relative to the arm circumference, can result in a spurious elevation of BP. (4) Marked brachial artery calcification, especially in older patients with heavily calcified arteries.(5) Clinician inertia, resulting in inadequate doses or irrational combinations of BP-lowering drug therapies.
Other causes of resistant hypertension
(1) Lifestyle factors, such as obesity or large gains in weight, excessive alcohol consumption, and high sodium intake.
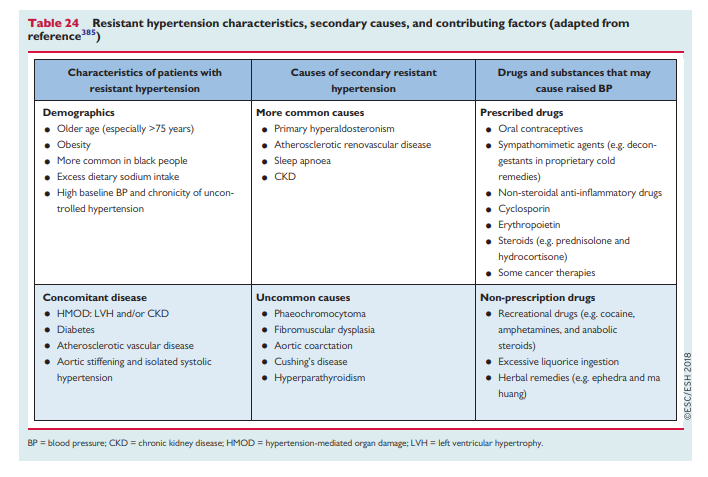
(2) Intake of vasopressor or sodium-retaining substances, drugs prescribed for conditions other than hypertension, some herbal remedies, or recreational drug use (cocaine, anabolic steroids, etc.) (see Table 24).
(3) Obstructive sleep apnoea (usually, but not invariably, associated with obesity).
(4) Undetected secondary forms of hypertension (see section 8.2).
(5) Advanced HMOD, particularly CKD or large-artery stiffening.
Resistant hypertension is associated with older age (especially >75 years), male sex, black African origin, higher initial BP at diagnosis of hypertension, highest BP ever reached during the patient’s lifetime, frequent outpatient visits, obesity, diabetes, atherosclerotic disease and HMOD, CKD, and a Framingham 10 year coronary risk score >20%.383,384
8.1.3 Diagnostic approach to resistant hypertension
Diagnosis of resistant hypertension requires detailed information about:
(1) The patient’s history, including lifestyle characteristics, alcohol and dietary sodium intake, interfering drugs or substances, and sleep history.
(2) The nature and dosing of the antihypertensive treatment.
(3) A physical examination, with a particular focus on determining the presence of HMOD and signs of secondary hypertension.
(4) Confirmation of treatment resistance by out-of-office BP measurements (i.e. ABPM or HBPM).
(5) Laboratory tests to detect electrolyte abnormalities (hypokalaemia), associated risk factors (diabetes), organ damage (advanced renal dysfunction), and secondary hypertension.
(6) Confirmation of adherence to BP-lowering therapy.
Patients should be screened for a secondary cause of hypertension, especially primary aldosteronism386 or atherosclerotic renal artery stenosis, particularly in older patients or patients with CKD.
Poor adherence to treatment should be considered, but its identification may be challenging in routine clinical practice.387 Some methods are easy to use but of limited value (e.g. standardized questionnaires), whereas others, such as drug screening of urine or blood, show considerable promise but are not yet widely available.388 Other methods include the measurement of BP after directly observed treatment intake,389 which has been used in clinical trials,390 but may be more
difficult to implement in routine clinical practice.8.1.4 Treatment of resistant hypertension
Effective treatment combines lifestyle changes (especially the reduction of sodium intake), discontinuation of interfering substances, and the sequential addition of antihypertensive drugs to the initial triple therapy. Ultimately, replacing all drugs by a simpler treatment regimen using SPC treatment is recommended to reduce pill burden and improve adherence to treatment. The optimal drug treatment of resistant hypertension has been poorly studied.
The most effective strategy seems to be additional diuretic treatment to decrease volume overload, together with the restriction of salt intake, particularly
in patients with CKD. BP control may be improved by increasing the dose of the existing diuretic or by switching to a more potent thiazide-like diuretic (chlorthalidone or indapamide).A loop diuretic should replace thiazides/thiazide-like diuretics if the eGFR is <30 mL/min. Although resistant hypertension may show a BP reduction if the existing diuretic dose is further increased, most patients require the administration of additional drugs.
There is growing evidence to suggest that the fourth-line treatment should involve a blockade of the biological effects of aldosterone through the use of MRAs391 (spironolactone up to 50 mg/day), as shown in the PATHWAY 2 study357 and supported by other studies and their meta-analysis.392–394
Not all patients will be able to tolerate spironolactone due to antiandrogenic side effects resulting in breast tenderness or gynaecomastia (in 6%), impotence in men, and menstrual irregularities in women.
Moreover, the efficacy and safety of spironolactone for the treatment of resistant hypertension has not yet been established in patients with significant renal impairment. As such, the use of spironolactone for resistant hypertension should usually be restricted to patients with an eGFR >_45 mL/min and a plasma potassium concentration of <_ 4.5 mmol/L. Moreover, electrolytes and eGFR should be monitored soon after initiation and at least annually thereafter.
On theoretical grounds, alternative additional diuretic therapy to spironolactone (when it is not tolerated due to androgen-like side effects) could include the MRA eplerenone (50 – 100 mg/day).
Amiloride (10 – 20 mg/day) has recently been shown to be as effective as spironolactone 25–50 mg daily) in reducing BP in thePATHWAY2 study.357 It is emphasized that the same cautions about the use of these agents should be considered in patients with reduced eGFR and baseline potassium levels >4.5 mmol/L.
The PATHWAY-2 study also evaluated bisoprolol (5 – 10 mg/day) or doxazosin modified release (4 – 8 mg/day) as alternatives to spironolactone. Neither was as effective as spironolactone, but they did reduce BP significantly vs. placebo when added to background treatment in resistant hypertension.310 Thus, bisoprolol and doxazosin have an evidence base for the treatment of resistant hypertension when spironolactone is contraindicated or not tolerated.
Direct vasodilators, such as hydralazine or minoxidil, are infrequently used because they may cause severe fluid retention and tachycardia.
New BP-lowering drugs (nitric oxide donors, vasopressin antagonists, aldosterone synthase inhibitors, neutral endopeptidase inhibitors, and endothelin antagonists) are all under investigation.388
Additional Resources: