If you are new to TEG and ROTEM, the YouTube video Episode 6: Your guide to TEG, ROTEM and the Medical Betamax Vs VHS Battle, (April 18, 2017 by Saud from The Surge: Trauma. Critical Care. Surgery) is a good introduction to the subject.
This post contains a link to and excerpts from A Simplified Treatment-Based Approach to TEG and ROTEM, 6/11/2018. By Adam Morcom, MD from EM Resident published by the Emergency Medicine Residents Association.*
*This site has a number of resources that are useful for all primary care physicians:
Since these are my study notes, I placed the whole article on this post for ease of review.
It’s becoming more common to use thromboelastography and rotational thromboelastometry in the ED. What’s your comfort level with TEG and ROTEM?
Case:
You receive a 40-year-old trauma patient who is hypotensive after a motor vehicle collision. As your team completes its secondary survey and FAST, you initiate massive transfusion protocol according to the standard 1:1:1 ratio of packed red blood cells to platelets to plasma. But what comes next? Are there additional tools you can use to help guide your resuscitation?
The use of viscoelastic hemostatic assays (VHAs) such as thromboelastography (TEG) and rotational thromboelastometry (ROTEM) are becoming increasingly common in the ED and trauma bay. While most EM physicians have likely heard of these diagnostic tests before, experience and comfort levels may vary widely when it comes to interpreting and ultimately using these test results to guide blood product transfusions and resuscitation endpoints.
Hades or Pluto?
Much like Greek and Roman mythology are filled with analogues—gods and goddesses who are eerily similar to one another but go by different names depending on which version of the story you read—so can ROTEM, TEG, and other VHAs be thought of as directly analogous to one another. The same properties are being measured, but are labeled with different names from one test to another. The advantage is that once you learn the specifics of a particular platform, it becomes very easy to apply the principles to any of its alternatives.
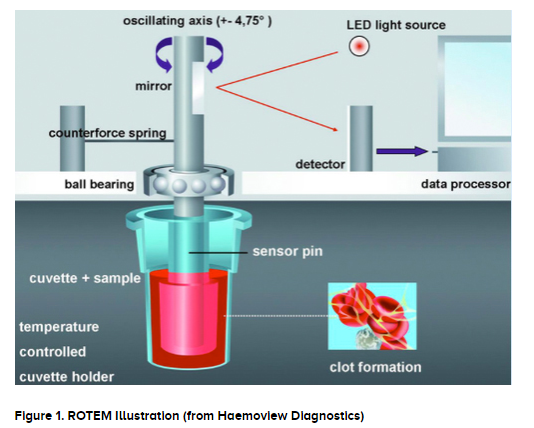
So what is actually happening in this assay? As blood clots form and strengthen, they exhibit increasing viscosity and elasticity. Physically speaking, both ROTEM and TEG involve the oscillating motion of a cylindrical shaft through a small sample of blood. As the blood forms into a clot, it exerts increasing resistance on the shaft. By measuring this resistance, we are able to track the strength of the forming clot over time. The results of TEG and ROTEM can be displayed as either a two-dimensional graph forming in real-time, or as a numerical list of pre-selected time intervals. Test results are often available in 30 minutes or less.
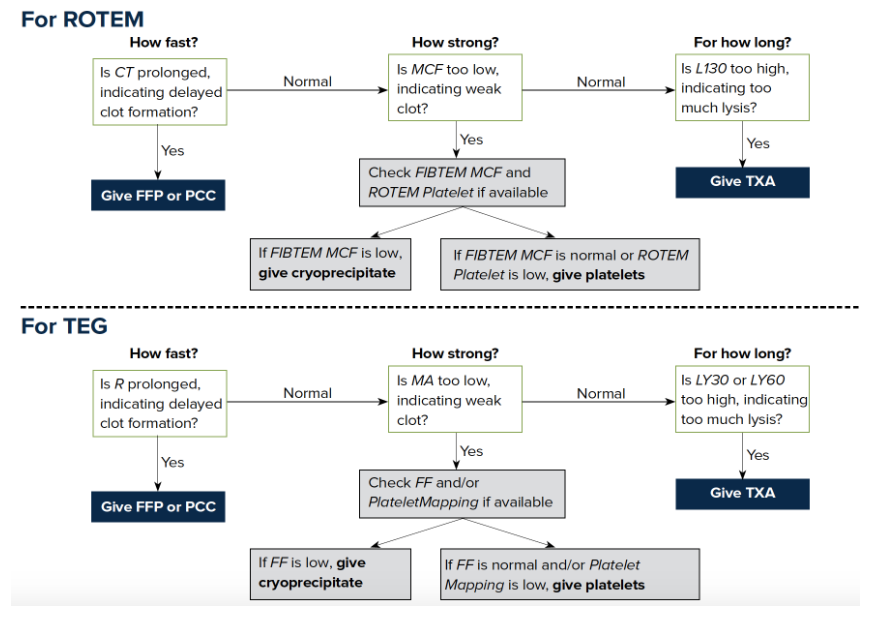
Both ROTEM and TEG provide a great deal of quantitative data; however, a simple approach to VHA-based treatment begins with focusing on 3 questions about clots:
- How fast?
- How strong?
- For how long?
How Fast?
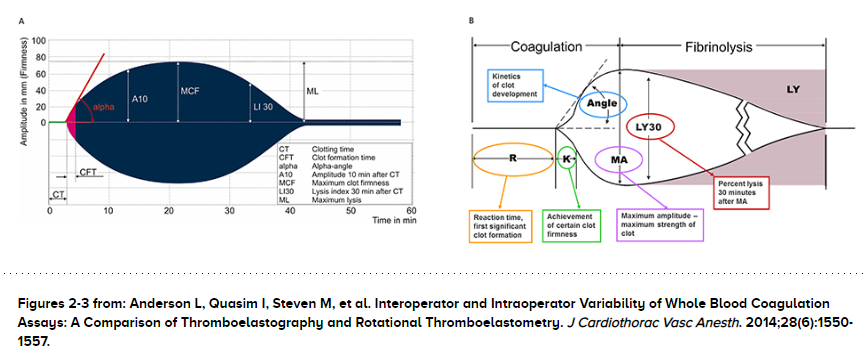
The first question to address is how quickly a new clot begins to form. This stage is represented by the linear portion on the left side of the graph (Figure 2), labeled clotting time (CT) for ROTEM (or specifically ROTEM’s EXTEM test, with re-agents added to isolate the extrinsic pathway of the coagulation cascade), or reaction time (R) for TEG. The time it takes a new clot to begin forming indicates the cumulative functionality of all the higher-level clotting factors within the coagulation cascade, leading up to the conversion of prothrombin to thrombin. Although there may be a great deal of complexity in this portion of the coagulation cascade, for the purposes of emergent bleeding, we can reduce this entire section to a single numerical value. Prolonged CT or R can be treated with fresh frozen plasma (FFP) or prothrombin complex concentrate (PCC).
How Strong?
How strong is the new clot once it’s formed? This should be thought of as a two-part question, because there are two major components that give a clot its strength: fibrin and platelets. You may recall that a clot is composed of a platelet plug, reinforced by cross-linked strands of polymerous fibrin chains. A deficiency in either fibrin or platelets will result in a pathologically weak clot. So how can we tell which of these two is deficient? With earlier generations of the technology, we would use a secondary test within either TEG or ROTEM to measure the contribution of fibrin directly, and then we would have to infer the contribution of platelets to clot strength indirectly. More recently, however, the companies that make TEG and ROTEM have released technologies capable of measuring platelet functionality directly, specifically TEG’s PlateletMapping® Assay or ROTEM® Platelet. These newer technologies may or may not be available at a given institution, and so it is still worth learning both the previous and newer methods. (Note that we are focused on platelet functionality, not simply platelet count.)
When assessing clot strength, we are looking at the highest amplitudes within the middle of the graph, namely the maximum clot formation (MCF) in ROTEM, or the maximum amplitude (MA) in TEG. If each of these values is normal, then there is likely no clot strength deficiency. However, if the clot is too weak overall, then we have to assess the two main components separately. Each platform has a devoted test to measure the contribution of fibrin to clot strength: the FIBTEM MCF in ROTEM, or the Functional Fibrinogen (FF) level in TEG. If the fibrin component is deficient, then we should replete it by TRAUMA giving cryoprecipitate. Using the older inference method, if the FIBTEM MCF or FF test is normal, but the overall clot strength (MCF or MA) is deficient, then we can infer that there is a deficiency in platelet functionality, and these should be repleted accordingly.
In some cases, both fibrin and platelets may be deficient. In order to detect this combination using the inference method, whenever you find and treat a deficiency in fibrin, you should run the test a second time. If the fibrin component has been corrected but the overall clot strength remains deficient, this indicates there must be a concurrent platelet deficiency, which should also be treated. Or alternatively, using the newer technologies, we can measure both fibrin and platelets individually and replete whichever is lacking.
How strong is the new clot once it’s formed? This should be thought of as a two-part question, because there are two major components that give a clot its strength: fibrin and platelets. You may recall that a clot is composed of a platelet plug, reinforced by cross-linked strands of polymerous fibrin chains. A deficiency in either fibrin or platelets will result in a pathologically weak clot. So how can we tell which of these two is deficient? With earlier generations of the technology, we would use a secondary test within either TEG or ROTEM to measure the contribution of fibrin directly, and then we would have to infer the contribution of platelets to clot strength indirectly. More recently, however, the companies that make TEG and ROTEM have released technologies capable of measuring platelet functionality directly, specifically TEG’s PlateletMapping® Assay or ROTEM® Platelet. These newer technologies may or may not be available at a given institution, and so it is still worth learning both the previous and newer methods. (Note that we are focused on platelet functionality, not simply platelet count.)
When assessing clot strength, we are looking at the highest amplitudes within the middle of the graph, namely the maximum clot formation (MCF) in ROTEM, or the maximum amplitude (MA) in TEG. If each of these values is normal, then there is likely no clot strength deficiency. However, if the clot is too weak overall, then we have to assess the two main components separately. Each platform has a devoted test to measure the contribution of fibrin to clot strength: the FIBTEM MCF in ROTEM, or the Functional Fibrinogen (FF) level in TEG. If the fibrin component is deficient, then we should replete it by TRAUMA giving cryoprecipitate. Using the older inference method, if the FIBTEM MCF or FF test is normal, but the overall clot strength (MCF or MA) is deficient, then we can infer that there is a deficiency in platelet functionality, and these should be repleted accordingly.
In some cases, both fibrin and platelets may be deficient. In order to detect this combination using the inference method, whenever you find and treat a deficiency in fibrin, you should run the test a second time. If the fibrin component has been corrected but the overall clot strength remains deficient, this indicates there must be a concurrent platelet deficiency, which should also be treated. Or alternatively, using the newer technologies, we can measure both fibrin and platelets individually and replete whichever is lacking.
For How Long?
Is the patient’s clot as durable as it needs to be, or is the clot breaking down sooner than it should? This is a question of fibrinolysis, represented by the rightward portion of the graph where the amplitude begins to decrease again, corresponding to the process by which plasminogen converts to the active plasmin and begins breaking down fibrin strands. This process occurs normally in healthy patients, however overactive plasmin causes hyperfibrinolysis, which is a treatable form of coagulopathy. To detect hyperfibrinolysis, you may examine the lysis index at 30 minutes (LI30) in ROTEM, or the lysis at 30 or 60 minutes (LY30, LY60) in TEG. If your bleeding patient’s clots are being lysed too quickly, you may treat with tranexamic acid (TXA). (Note that this targeted treatment differs from the guidelines based on the CRASH2 trial, which advises that empiric TXA must be given within the first 3 hours of injury to confer mortality benefit. However, bleeding patients with an identified hyperfibrinolysis represent a different patient population than that of CRASH2, and therefore not subject to the same 3-hour window.)
See the article for the following sections at the end of the article:
- What About Those Other Parameters, Not Discussed Here?
- What About Patients Taking NOACs?
- When to Use TEG or ROTEM?