In this post I link to and excerpt from Emergency Medicine Cases’ ECG Cases 1: Missed Ischemia-Never Trust The ECG Computer Interpretation. Written by Jesse McLaren; Edited by Anton Helman. September 2019.
All that follows is from Dr. McLaren’s post.
In this ECG Cases – Missed Ischemia – Never Trust the ECG Computer Interpretation, we review ECGs from 7 patients presenting to the ED with chest pain, all of whom had a computer interpretation as “normal.” And guess what…they all show acute ischemia! Can you see what the computer couldn’t?
ECGs read as ‘normal’ by the computer
Automated interpretation has high rates of error for detecting ischemia, up to 42% for STEMI.[1] But what about those ECGs read as “normal”? A 2017 study concluded that “triage ECGs identified by the computer as normal are unlikely to have clinical significance that would change triage care. Eliminating physician review of triage ECGs with a computer interpretation of normal may be a safe way to improve patient care by decreasing physician interruptions.” [2]
But this was based on only 4 months of triage ECGs collected at a single centre with a low incidence of STEMI. A critical response explained both the shortcomings of the study, and a different approach to “normal” ECGs:
“Using non-blinded expert review rather than outcome as a reference standard precludes any meaningful conclusion about triage ECGs…A sample size of 855 has no chance of generating a meaningful conclusion about the reliability of computer ‘Normal.’…Physicians should take steps to develop their skills in detecting subtle signs of myocardial ischemia, and computerized interpretation algorithms should state ‘No abnormalities detected’ rather than ‘Normal ECG.’ ” [3]
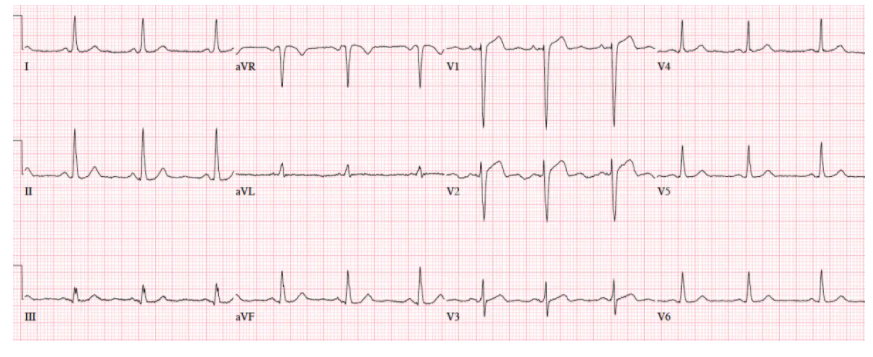
Patient 1. 65yo with hours of chest pain. No prior ECG
Patient 1. ischemic ST morphology
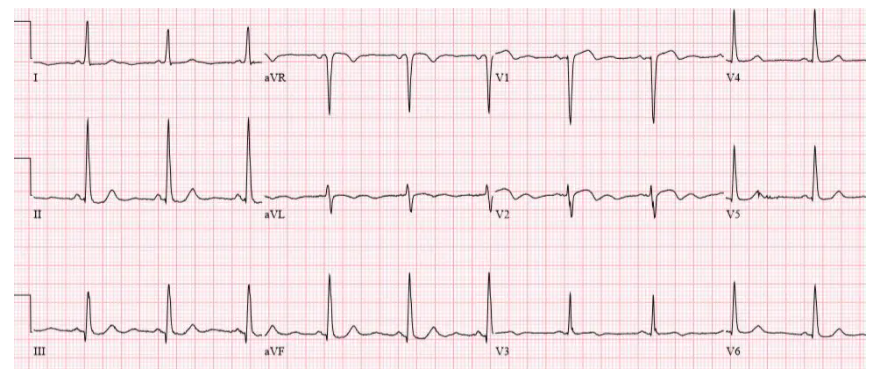
NSR, normal conduction/axis/R wave, no hypertrophy. Mild ST elevation in V1-2 which could be normal, but the morphology is not: ST is convex in V2 and straight in V3. Plus there’s an inverted U wave in V2, another marker of LAD occlusion. When trop returned positive an hour later, repeat ECG below showed further convex ST in V1-2 and terminal T wave inversion, and cath lab was activated: 100% mid LAD occlusion