In this post I link to and excerpt from Emergency Medicine Cases’ ECG Cases 2: Early Repolarization or Anterior STEMI? Written by Jesse McLaren; Peer Reviewed and edited by Anton Helman, October 2019.
All that follows is from Dr. McLaren’s post.
In this ECG Cases blog we present ECGs from 7 patients who presented with chest pain and mild anterior ST elevation. Can you identify which were early repolarization and which were anterior STEMI?
Early repolarization vs anterior STEMI
According to the latest guidelines, anterior STEMI is diagnosed when there is new ST elevation at the J point in two contiguous anterior leads of 1mm, except for V2-3 which need 1.5mm in women, 2mm in men 40 and older, and 2.5mm in men <40. But this is neither sensitive nor specific for the underlying pathology it is meant to diagnose: occlusion of the left anterior descending (LAD) coronary artery. Neither ST amplitude nor morphology reliably differentiate between LAD occlusion and early repolarization. As Stephen Smith explained,
“The 2 entities may be difficult to distinguish from each other for several reasons. First, upward ST-segment concavity, usually associated with normal ECG results, is also present in 30% to 40% of anterior STEMI (due to left anterior descending artery occlusion), especially early after onset of symptoms. Moreover, 30% to 40% of anterior STEMIs have borderline ST-segment elevation (absence of 2 consecutive leads with at least 2mm of ST-segment elevation), and 20% may have upward concavity and borderline ST-segment elevation. Conversely, most benign ECGs have at least 1mm of ST-segment elevation in right precordial leads.” [1]
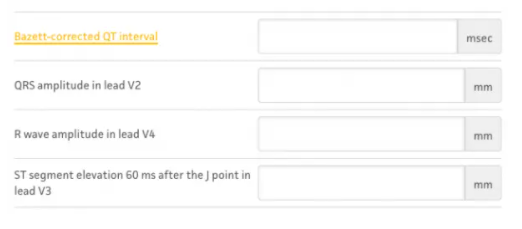
Dr. Smith has developed a formula for differentiating early repolarization from subtle LAD occlusion, in cases where there is at least 1mm of STE in at least 1 anterior lead. It examines ST elevation relative to the QRS complex (higher in early repolarization) and QT interval (shorter in early repolarization).[2] It is available on MD-calc, and begins with important BER exclusion criteria:
In this ECG Cases blog we present ECGs from 7 patients who presented with chest pain and mild anterior ST elevation. Can you identify which were early repolarization and which were anterior STEMI?
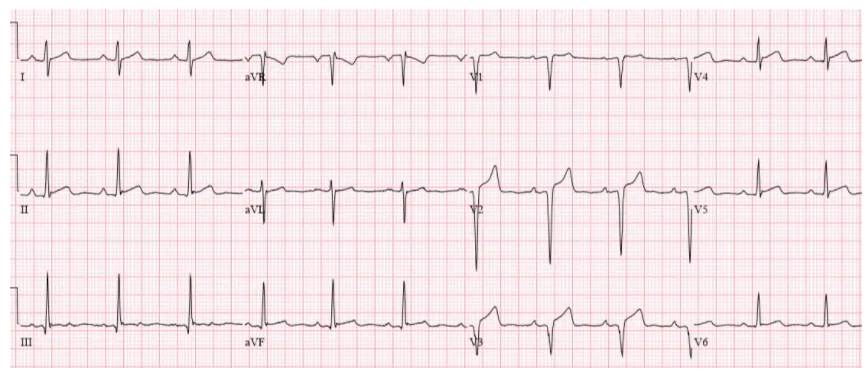
Patient 1: 30yo smoker with chest pain radiating to the arm
NSR, normal conduction/axis, no hypertrophy. Concave ST elevation V2-4 without reciprocal change, which was assumed to be from early repolarization because of the patient’s young age. But V2-3 have Q waves and total loss of R waves. (While Q waves can be seen in old MI, V3 has T/QRS > 0.36, which differentiates anterior STEMI from LV aneurysm [3]; more cases on this in a subsequent post). When trop came back at 3,000 cath lab was activated: 95% mid-LAD occlusion. Discharge ECG shows LV aneurysm morphology with T/QRS < 0.36.