In this post I link to and excerpt from Emergency ECG Cases 15: Tall R Wave in V1. Written by Jesse McLaren; Peer Reviewed and edited by Anton Helman, November 2020.
Note to myself when reviewing: First review the notes below from Dr. McClaren’s post and then go to the post itself to test myself by reviewing the ten ECGs he has provided for us.
All that follows is from Dr. McClaren’s post:
In this ECG Cases blog we look at 8 patients who presented with tall R wave in V1
Eight patients presented with ECGs that had a tall R wave in V1
Tall R wave in V1-2
As a review article by Dr. Mattu explained,
“In the normal heart, the general direction of ventricular depolarization is in a right-to-left, downward direction because of the larger mass of the left ventricle compared with the right ventricle. This results in a characteristic appearance of the QRS complex in lead V1 of the ECG, the rS configuration. The initial small R wave (symbolized as ‘r’ to denote its small size) occurs because of septal depolarization from left to right. The subsequent larger S wave (symbolized as ‘S’ to denote its larger size) occurs because of the dominant effect of the left ventricle. Tall R waves in lead V1 (tall RV1), defined as an R/S ratio equal to or greater than 1, is not an infrequent occurrence the emergency department patients. However, this ECG finding exists as a normal variant in only 1% of patients. Physicians should therefore be familiar with the differential diagnosis for this important QRS configuration.”[1]
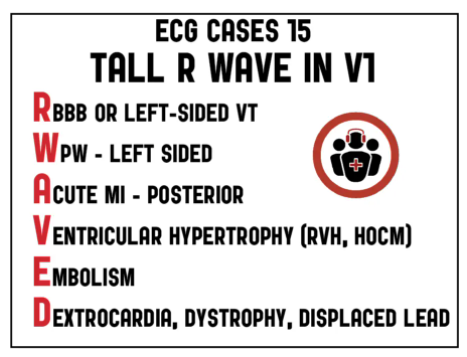
Tall R waves in V1 can be caused by abnormal electrical conduction (RBBB or left-sided VT, which slowly spreads across the right ventricle, or a left-sided accessory pathway), loss of posterior myocardium (old or acute posterior MI) or chronic anterior hypertrophy (HCM), chronic or acute RV strain (RVH, PE), congenital anomalies (dextrocardia or dystrophy), misplaced leads, or a normal variant (persisting juvenile pattern). This differential can be remembered by the mnemonic R-WAVED
- RBBB (RsR’, QRS>120, wide S in V6, secondary repolarization abnormalities in anterior leads) or left-sided VT/ventricular ectopy
- WPW left sided pathway: PR<120, QRS>110, delta wave, tall R in V1-2 with discordant ST/T wave changes
- Acute MI – posterior: tall R wave V1 or V2 and ST depression +/- inferior or lateral ST elevation +/- posterior ST elevation
- Ventricular hypertrophy: RVH (R/S >1 in V1 and <1 in V6, right axis deviation, secondary repolarization changes) or HCM
- Embolism: +/- sinus tach, RBBB, S1Q3T3, anterior/inferior TWI
- Dextrocardia (negative P wave, reversed R wave progression), dystrophy, or displaced leads (eg V1 and V3 switched)
These causes are not mutually exclusive but can co-exist, which can be challenging. Because many causes of tall R waves in V1 are caused by abnormal depolarization (eg RBBB, RVH, WPW, HCM), they produce abnormal repolarization changes that can mask or mimic acute ischemia. Knowing that RBBB causes discordant anterior ST depression and T wave inversion can help identify occlusion MI in the presence of RBBB by either concordant ST elevation (anterior MI) or disproportionate ST depression (posterior MI). In terms of WPW, “some pathways may only carry impulses in the retrograde manner and thus are ‘concealed’ conduction pathways; these pathways are ‘silent’ – normal PR interval and QRS complex and the absence of the Delta wave – on the resting 12 lead ECG. In other cases, the bypass tracts conduct intermittently, depending upon other factors such as cardioactive medication use, physiological stressors with catecholamine release, the development of coronary ischemia, and normal aging.”[2]
Now go to Dr. McClaren’s post and test yourself against his six ECGs.
And when you analyze the ECG, use the H E A R T S template to analyze the ECG.
So, the first time through, I’m going to go thru the H E A R T S template answer for each of the six ECGs. So go to the post and to the second six ECGs after Dr. McClaren’s great review notes. I’ll list the ten H E A R T S template answers for my review.
Returning to Dr. McClaren’s post:
Eight patients presented with ECGs that had a tall R wave in V1
Case 1: 70yo with recurring syncope at rest
Case 1: syncope from bifascicular block and borderline first degree heart block
- Heart rate/rhythm: sinus bradycardia
- Electrical conduction: RBBB + LAFB, borderline first degree heart block
- Axis: left axis from LAFB
- R wave: tall R in V1 from RBBB, poor R wave progression from LAFB
- Tension: no hypertrophy
- ST/T changes: nonspecific
Impression: recurring syncope at rest with bifascicular block and borderline first degree heart block. Labs normal, admitted for pacemaker.