In this post I link to and excerpt from Emergency Medicine Cases’ ECG Cases 4: Lateral STEMI or Occlusion MI? Written by Jesse McLaren; Peer Reviewed and edited by Anton Helman. December 2019.
All that follows is from Dr. McLaren’s post.
In this ECG Cases blog we look at seven patients with potentially ischemic symptoms and subtle ECG changes in the lateral leads. Which had acute coronary occlusion? Introducing the concept of Occlusion MI – a paradigm shift in ECG diagnosis of MI…
Lateral STEMI vs Occlusion MI
The left ventricular lateral wall (represented by leads I, AVL, V5-6), is supplied by the diagonal branches of the left anterior descending artery and the circumflex artery and its branches. Depending on the vessel, acute coronary occlusion can be anterolateral (LAD), posterolateral +/- inferior (circumflex), or isolated lateral (LAD diagonal branch or circumflex obtuse marginal branch).
But the lateral wall is relatively electrocardiographically silent, so acute coronary occlusion can be subtle. Lateral STEMI criteria requires at least 1mm of ST elevation in at least two contiguous lateral leads; those not meeting this threshold are designated as NSTEMI and receive delayed reperfusion. But in a study of more than 500 patients with persisting ischemic symptoms and any amount of ST elevation, 18% of acute coronary occlusions had less than 1mm of ST elevation (including 35% of circumflex occlusions), though they had the same mortality rates. But two-thirds of subtle occlusions had reciprocal ST depression, indicating that other aspects of the ECG interpretation besides magnitude of ST segment elevation can help diagnosis.[1] As a database of more than 30,000 NSTEMI patients found, “Approximately one-quarter of patients with NSTEMI had an occluded culprit vessel at the time of angiography. Of these, 66% occurred in the posterolateral distribution, demonstrating the limitations of the current diagnostic approach to acute coronary syndromes, which relies heavily on STEMI/NSTEMI dichotomization for early treatment decisions.”[2]
As a consequence, a new paradigm is emerging, which uses insights from angiography and advances in ECG interpretation to identify the underlying condition that STEMI criteria fails to represent: Occlusion MI (OMI). As Pendell Meyers and Stephen Smith explain, “Twenty-five percent of patients diagnosed with NSTEMI have complete occlusion of the culprit vessel found on delayed angiogram, and a similar percentage of our cardiac catheterization lab activations turn out to be false positives. These false negatives [STEMI(−) OMI] are denied the opportunity to benefit from reperfusion therapy, while the false positives [STEMI(+) non-ACS] may receive harm from unnecessary cardiac catheterization…which has led us to propose a paradigm shift from the STEMI vs. Non-STEMI paradigm to one we call Occlusion MI vs. non-Occlusion MI (OMI vs. NOMI) paradigm.” [3]
Even when ECGs don’t meet STEMI criteria, NSTEMI guidelines also call for immediate invasive (within 2hr) reperfusion for patients with:
- refractory angina
- signs or symptoms of HR or new or worsening mitral regurgitation
- hemodynamic instability
- recurrent angina or ischemia at rest or with low-level activities despite intensive medical therapy
- sustained VT or VF [4]
In this ECG Cases blog we look at seven patients with potentially ischemic symptoms and subtle ECG changes in the lateral leads. Which had acute coronary occlusion? Introducing the concept of Occlusion MI – a paradigm shift in ECG diagnosis of MI…
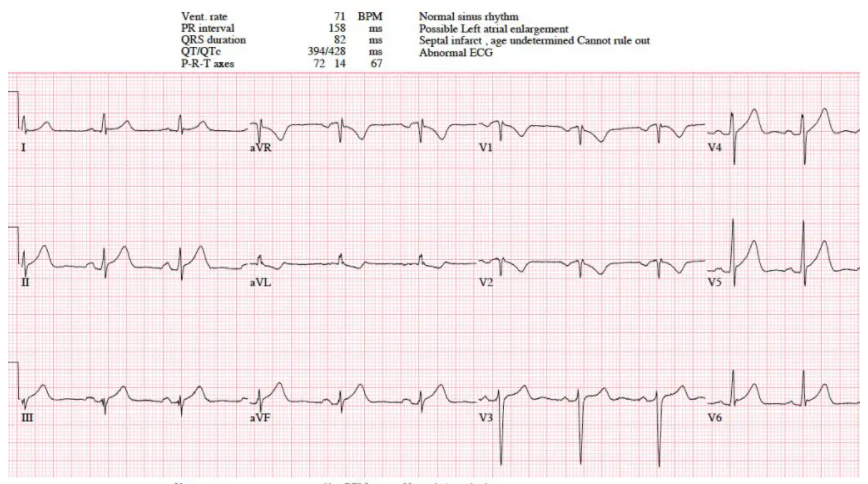
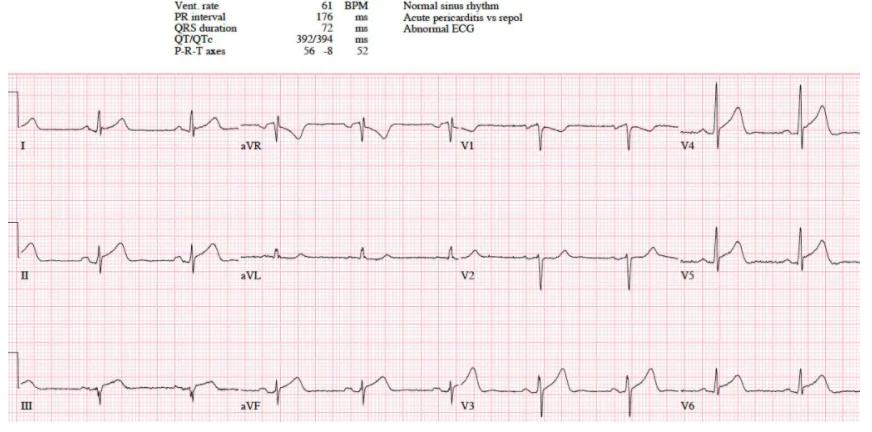
Patient 1: 50yo with one hour chest pain and nausea, serial ECGs:
Patient 1: inferoposterolateral STEMI(+)/OMI(+)
NSR, normal conduction/axis/R wave progression, no hypertrophy. First ECG has V2 placed too high, giving inverted P/T waves, which is corrected on second ECG. There’s 1mm inferolateral ST elevation that meets STEMI criteria but which can also be seen with pericarditis. But there are also hyperacute T waves (most obviously inferiorly, where they are larger than their preceding R wave) , and dynamic reciprocal changes in aVL (which is very specific for inferior MI). STE in III also becomes convex, and there is ST depression in V2 concerning for posterior extension. Cath lab activated: circumflex occlusion. Follow-up ECG: resolution of ST elevation, hyperacute T waves, reciprocal change in AVL and ST depression in V2.