In this post I link to and excerpt from 2015 ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension: The Joint Task Force for the Diagnosis and Treatment of Pulmonary Hypertension of the European Society of Cardiology (ESC) and the European Respiratory Society (ERS): Endorsed by: Association for European Paediatric and Congenital Cardiology (AEPC), International Society for Heart and Lung Transplantation (ISHLT) [PubMed Abstract] [Full-Text HTML] [Access Full-Text PDF from the HTML link]. Eur Heart J. 2016 Jan 1;37(1):67-119. doi: 10.1093/eurheartj/ehv317. Epub 2015 Aug 29.
Comment in
Similar articles
Cited by 1,367articles
All that follows is from 2015 ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension:
3. Definitions and classifications
3.1 Definitions
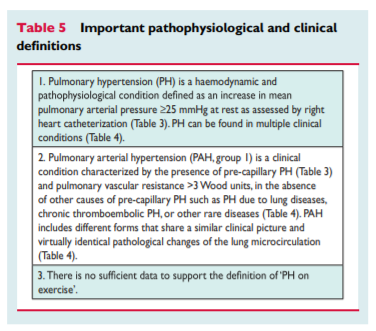
PH is defined as an increase in mean pulmonary arterial pressure (PAPm) ≥25 mmHg at rest as assessed by right heart catheterization (RHC).1 Available data have shown that the normal PAPm at rest is 14+3 mmHg with an upper limit of normal of approximately 20 mmHg.1,2 The clinical significance of a PAPm between 21 and 24 mmHg is unclear. Patients presenting with a pulmonary artery pressure (PAP) in this range should be carefully followed when they are at risk for developing PAH [e.g. patients with connectivetissue disease (CTD) or family members of patients with heritable PAH (HPAH)].1
Due to the lack of reliable data that define which levels of
exercise-induced changes in PAPm or PVR have prognostic implications, a disease entity ‘PH on exercise’ cannot be defined and should not be used.1 A recent retrospective study has proposed a definition of PH on exercise with the combination of PAPm and total PVR data, but no outcome prospective validation has been provided.3The term PAH describes a group of PH patients characterized
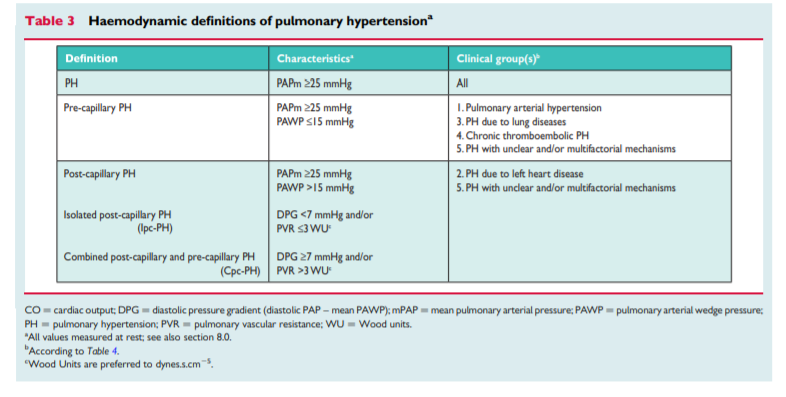
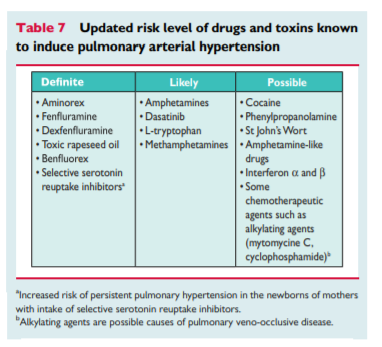
haemodynamically by the presence of pre-capillary PH, defined by a pulmonary artery wedge pressure (PAWP) ≤15 mmHg and a PVR > 3 Wood units (WU) in the absence of other causes of precapillary PH such as PH due to lung diseases, CTEPH or other rare diseases.1According to various combinations of PAP, PAWP, cardiac output (CO), diastolic pressure gradient (DPG) and PVR, assessed in stable clinical conditions, different haemodynamic definitions of PH are shown in Table 3 together with their corresponding clinical classification (Table 4).1,4 The reasons for the updated definitions of post-capillary PH are reported in the specific section (8.0).
5. Pulmonary hypertension diagnosis
5.1 Diagnosis
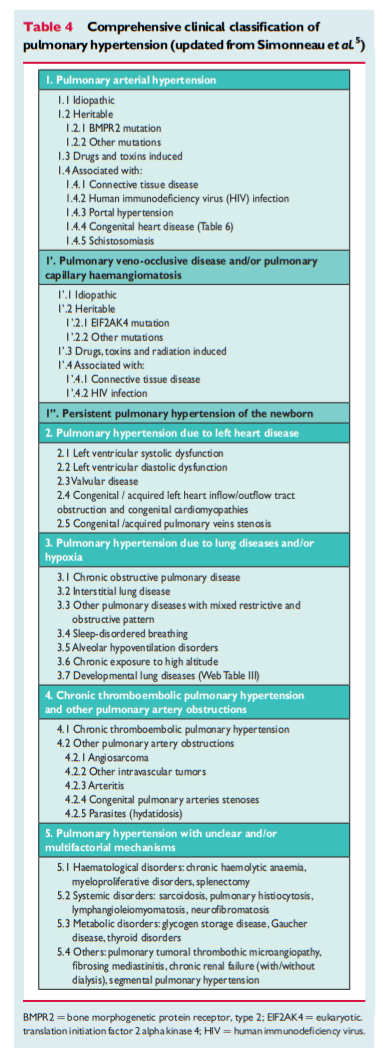
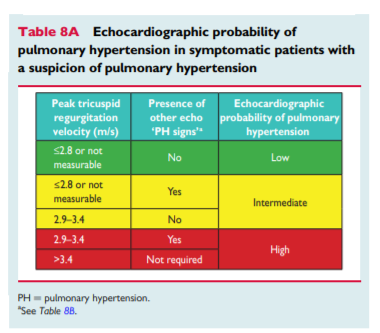
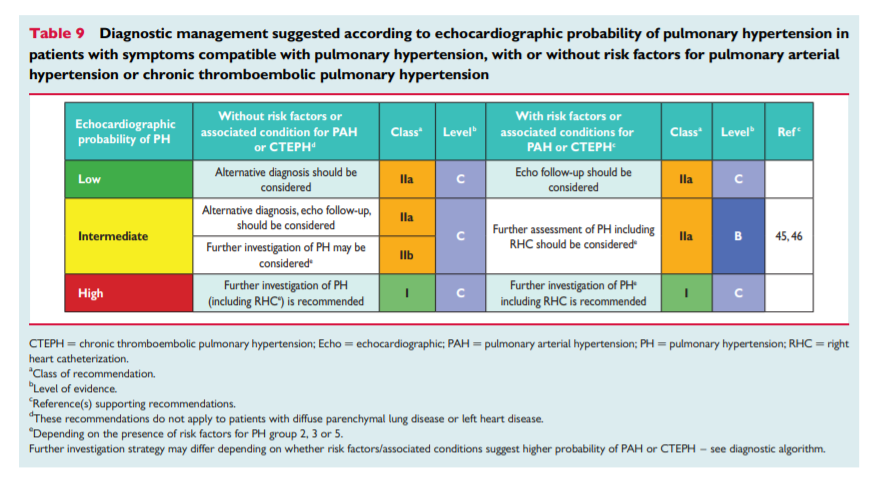
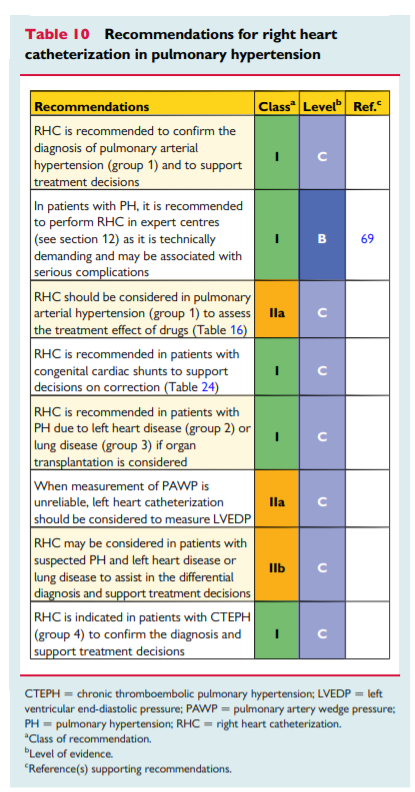
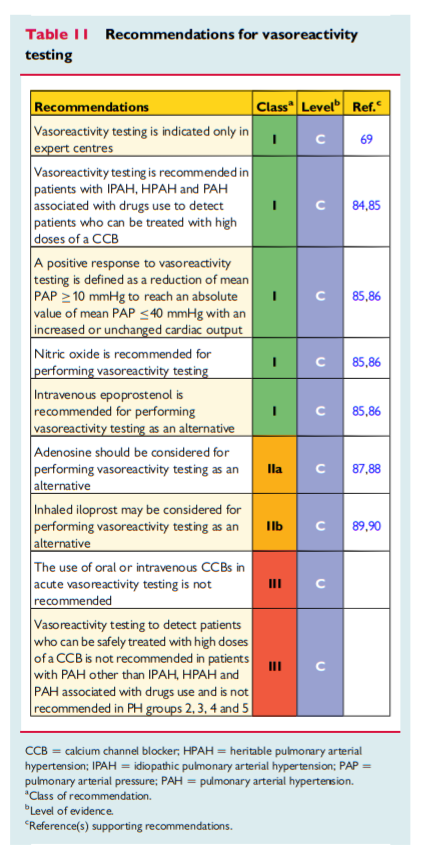
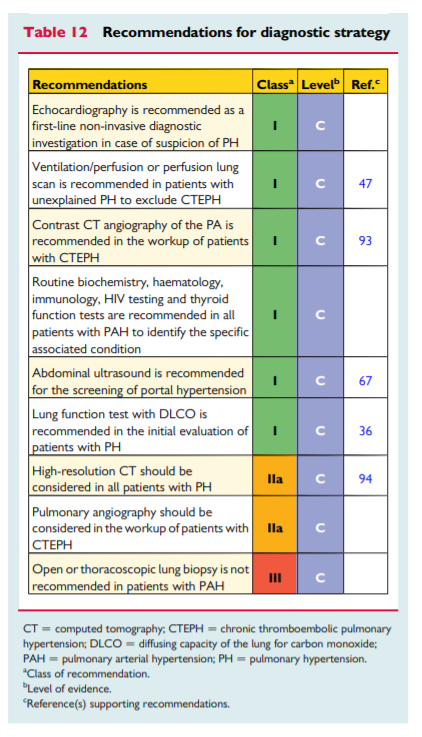
The diagnosis of PH requires a clinical suspicion based on symptoms and physical examination and review of a comprehensive set of investigations to confirm that haemodynamic criteria are met and to describe the aetiology and the functional and haemodynamic severity of the condition. The interpretation of these investigations requires, at the very least, expertise in cardiology, imaging and respiratory medicine and may best be discussed at a multidisciplinary team meeting. This is particularly important for identifying patients who may have more than one cause of PH. The main cause of PH should be identified according to the clinical classification in Table 4. [Above] An algorithm for reaching a diagnosis is shown in Figure 1. [Above]