In this post I link to and excerpt from ADHD in Children and Youth: Part 2 – Treatment – CPS Podcast from PedsCases.
The above podcast is based upon ADHD in children and youth: Part 2-Treatment [PubMed Abstract] [Full Text HTML] [Full Text PDF]. Paediatrics & Child Health, 2018, 462–472 from The Canadian Paediatric Society.
Here are excerpts from the podcast:
This podcast is part 2 of a 3-part series on ADHD in children and youth based on the 2018 CPS Statement on ADHD. It will cover the management of ADHD, including non-pharmacologic treatment, when to consider medical intervention, and pharmacologic options. This series was developed by Renée Lurie, a third-year medical student from the University of Ottawa, in collaboration with the authors of the statement: Drs. Stacey Bélanger, Mark Feldman, and Brenda Clark from the Universities of Montreal, Toronto, and Alberta respectively.
Related Content
- Podcast: ADHD in Children and Youth: Part 1 – Etiology, Diagnosis, and Comorbidity – CPS Podcast
- Podcast: ADHD
- Podcast: Developmental Assessment
- Case: School difficulties in a 7-year-old female
Introduction
This is part two of a three-part series based on the 2018 CPS Statement on Attention Deficit and Hyperactivity Disorder. This podcast will discuss the new CPS statement, ADHD in children and youth: Part 2 – Treatment.*
*What follows is from the CPS statement above:
NONPHARMACOLOGICAL INTERVENTIONS FOR ADHD
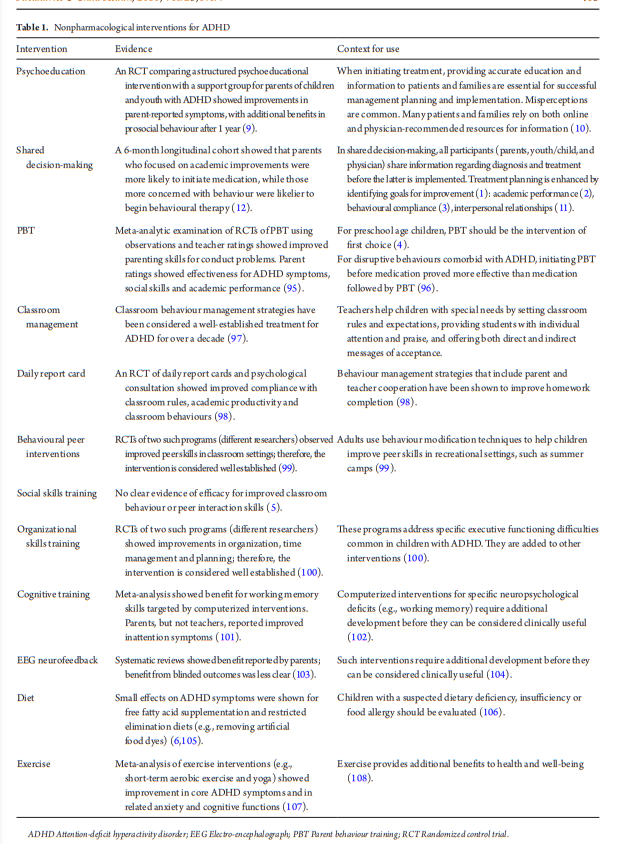
Current ADHD guidelines recommend including nonpharmacological interventions as part of treatment planning for children and adolescents with ADHD (1–3).
Table 1 summarizes nonpharmacological interventions for ADHD.
INITIATING TREATMENT
For children with ADHD younger than 6 years of age, evidence is robust that first-line intervention should be parent behaviour training (4). Overall evidence for the effectiveness of psychostimulants is weak, and Health Canada has not approved their use in this age group. Medication works primarily on core ADHD symptoms and should be considered for children aged 6 years and older (5–7).
However, more than one-half of children with ADHD have psychiatric and developmental comorbidities (8). For this reason, nonpharmacological interventions (Table 1) should be considered routinely as part of comprehensive ADHD care, with
specific goal-setting to improve compliance, academic performance, and quality of life. Psychoeducation around optimal supportive care should be available for all patients and families of children and youth with ADHD (9,10).
INITIATING AND MONITORING STIMULANT MEDICATIONS
Initial titration and monitoring to evaluate the benefits and AEs
of ADHD medication should include using standardized questionnaires (33–35) and checklists (33,34) (www.cps.ca/en/
tools-outils/mental-health-screening-tools-and-rating-scales).
Parents and older children can provide baseline observations
regarding symptom severity and potential AEs. Baseline and
follow-up teacher observations are also essential for monitoring
treatment response (36).
And now returning to the PedsCases ADHD Part 2 transcript:
Management:
ADHD treatment should comprise of a combination of pharmacological and nonpharmacological interventions. As many of these children have other psychiatric and developmental conditions, non-pharmacologic interventions are extremely beneficial to ensure the patient has a well-rounded care plan.
As there is a large range of non-pharmacologic interventions, treatment plans must be individualized to the patient’s goals of care. Non-pharmacologic treatments should always be implemented first, or in conjunction with medications, if indicated. Non-pharmacologic interventions vary from those implemented in and outside of the school. At school, classroom
interventions such as establishing routines and using visual cues, organizational skills training and daily report cards can be implemented. Outside of school, interventions include behavioural techniques focused on peer interactions and parent behaviour training. It is also important to manage the child’s overall well-being through proper diet, sleep and exercise.Now onto pharmacologic interventions!
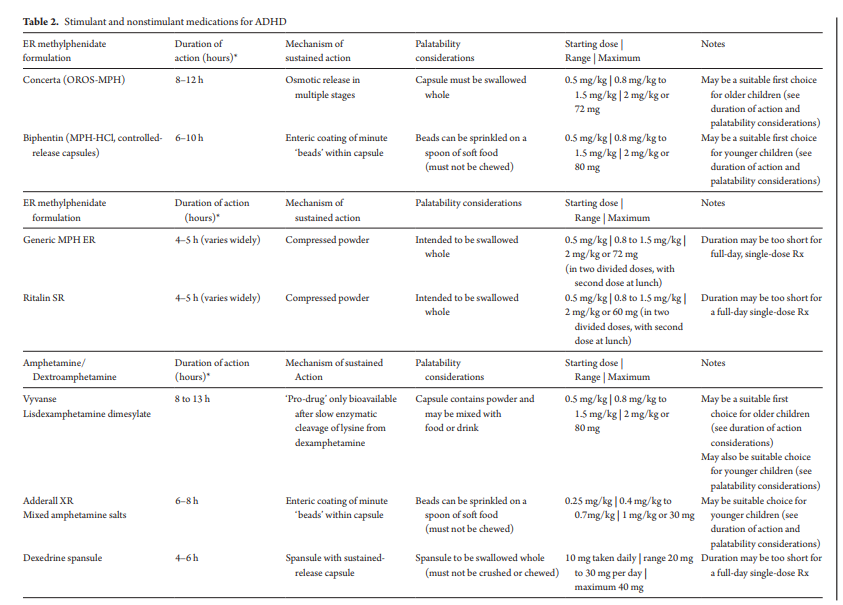
The most effective medications used to treat ADHD are stimulants. These include dextroamphetamine-based (Adderall, Vyvanse) and methylphenidate-based (Biphentin, Concerta, Ritalin) medications. Stimulants can be very effective in both children and youth. For example, studies have shown improvements in school work productivity, decision making, fewer injuries needing ER visits, and better driving performance in adolescents1-5
Prior to starting medications, it is important to set goals or outcomes with the patient. These will help direct the treatment plan. The goals should be focused on symptom reduction and
improving function, whether that be at school, in relationships or becoming more independent. As well, to track the patient’s responsiveness to medications, standardized checklists should be
used prior to and during treatment. These checklists should be completed in two or more settings, and must include involvement from the child’s school. Examples of validated tools
include the ADHD Rating Scale IV and the Conners Rating Scale6The difference between the two main stimulant classes – methylphenidate and dextroamphetamine – is minimal. The choice of medication should depend on its effect, cost and administration. Stimulants are available in short-, intermediate-, and long-acting preparations.
If a medication change is required, before switching to a non-stimulant medication, another formulation of stimulant in the same class or an entirely different class of stimulant should be
tried.Non-Stimulant Medications:
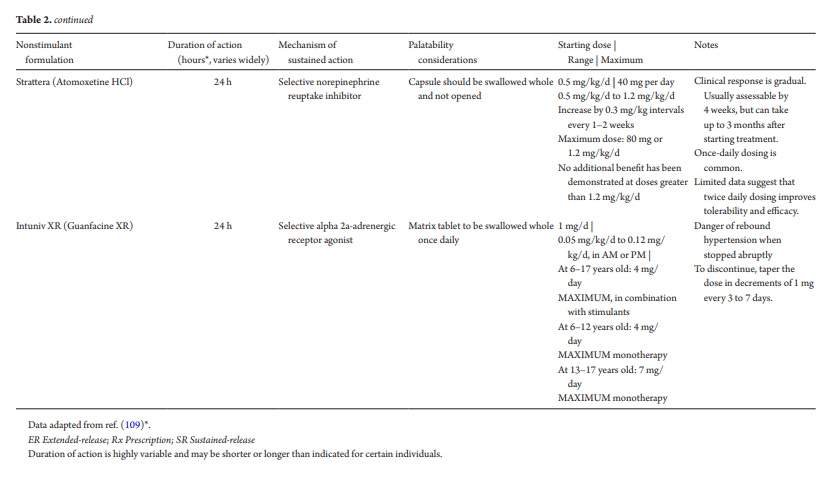
Although not first-line (and with a smaller treatment effect size), it is also important to discuss the two, long-acting non-stimulant medications, Atomoxetine – a selective norepinephrine reuptake inhibitor and Guanfacine XR – an alpha adrenergic drug. They are approved for children aged 6 to 17 years. These medications are given as add-ons to stimulants or when stimulants are contraindicated, ineffective or not tolerated. As their mechanism of action differs from that of a stimulant, they are less likely to be abused as their effect time is not as quick as a stimulant. If a stimulant is chosen for these individuals, a long-acting formulation is preferred.
Non-stimulants generally last up to 24 hours and are usually once-daily dosing.Most children without comorbid conditions are usually diagnosed and treated by their primary care provider. If the child has comorbid psychiatric, neurological or medical conditions or is still struggling after a trial of stimulants or non-stimulants, then a referral to or a consultation with
specialist should be considered8. A referral can be made not only to specialist physicians but also psychologists, occupational therapists, social workers, and other health care professionalsKey points learned:
1. ADHD is best managed with a combination of non-pharmacologic and pharmacologic interventions.
2. Non-pharmacologic interventions should focus on the child, school and parents. Examples of these include exercise, classroom accommodations and parent behaviour training.
3. When medications are required, stimulants are first line. If a stimulant is not effective in reducing symptoms or has adverse effects, changing the dose or using another formulation of stimulant in the same class or an entirely different class of stimulant should be tried. If there is still a large burden of symptoms or side effects, a nonstimulant medication can be prescribed.
4. A referral to a specialist may be helpful in terms of management if the child has
comorbid conditions or has tried multiple medication trials with minimal improvements.
Thank you for listening! Stay tuned for part 3 of our series where we will discuss the
assessment and treatment of children with ADHD and common comorbidities!