In this post I link to and excerpt from Dr. Josh Farkas‘ Internet Book of Critical Care [Link is to Table Of Contents], Approach To Stupor and Coma. March 22, 2021
Note to myself: In future reviews, just go to Dr. Farkas’ chapter to review. The excerpts are not complete and are just to help me remember.
All that follows is from the chapter.
CONTENTS
- Definitions
- Causes of stupor & coma
- History
- Coma neuro exam
- Coma syndromes
- Tests & investigations
- Airway management
- Emergent therapies to consider
- Pseudocoma
- Overview
- Podcast
- Questions & discussion
- Pitfalls
- PDF of this chapter (or create customized PDF)
definitions
basics
- Coma is defined as a state of being unawake (closed eyes), unaware, and unarousable.
- Stupor lacks a clear definition, but usually refers to substantially impaired mental status with preservation of some responsiveness to painful stimuli.
- Locked-in syndrome usually results from pontine lesions. Patients are awake and cognitively intact, but paralyzed (only with the ability to blink or move their eyes vertically). It is essential to promptly recognize locked-in syndrome and differentiate this from coma or stupor.
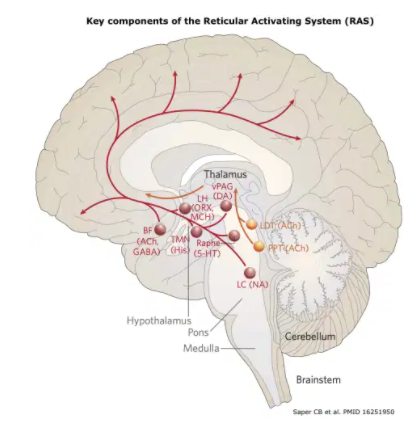
- Coma results from disruption of pathways from the ascending Reticular Activating System. This system originates in the tegmentum of the upper pons and midbrain, projects to the hypothalamus and bilateral thalami, and subsequently diverges widely throughout the bilateral cortexes.
- For a lesion to cause coma, it must have one of the following locations:
- (1) Dorsolateral upper-mid pontine lesion
- (2) Paramedian upper midbrain lesion
- (3) Bilateral thalamic injury
- (4) Diffuse bihemispheric damage
- ⚠️ Coma cannot be attributed to a unilateral cortical lesion alone.(33218655) For example, in order for a unilateral cortical lesion to cause coma it must cause a herniation syndrome that results in damage to the upper midbrain.
causes of stupor & coma
vascular
- Intracranial hemorrhage:
- Subarachnoid hemorrhage.
- Thalamic or Pontine hemorrhage.
- Ischemic stroke(s)
- i) Most commonly, basilar artery stroke.
- ii) Severe multifocal infarction (e.g., due to endocarditis).
- Hypertensive encephalopathy, a.k.a. posterior reversible encephalopathy syndrome (PRES).
- Venous sinus thrombosis (thrombosis of the straight sinus may cause bilateral thalamic dysfunction).
infection
- Meningitis.
- Encephalitis (most notably due to HSV or VZV).
- Brain abscess or subdural empyema that exerts mass effect.
severe metabolic derangements
- Hypoxic/anoxic brain injury.
- Hypercapnia (e.g., pCO2 typically over ~80-100 mm).
- Hypothermia or hyperthermia (e.g., temperature <28C or >40C).(27741988)
- Hypoglycemia (glucose below ~40 mg/dL or ~2.2 mM).(20130300)
- Hyperglycemia (rapid rise in glucose above ~900 mg/dL or ~50 mM).(20130300)
- Hyponatremia (e.g., sudden drop below ~110 mM).(20130300)
- Hypernatremia (e.g., sudden rise above ~160 mM).(20130300)
- Hypercalcemia (e.g., ionized calcium above ~3.5 mM).(20130300)
- Hepatic encephalopathy.
- Severe hyperammonemia.
- Uremia.
- Myxedema coma.
- Wernicke’s encephalopathy.
toxicologic
- Opioids.
- Alcohols (ethanol, methanol, ethylene glycol).
- Sedatives, including baclofen.
- Serotonin syndrome.
- Sympathomimetic intoxication.
- Salicylate poisoning.
- Lithium.
- Anticholinergics, including tricyclics.
- Carbon monoxide
trauma/surgery
- Hematoma (subdural, epidural, or parenchymal).
- Diffuse axonal injury.
- Fat emboli syndrome.
nonconvulsive status epilepticus
psychiatric
- Functional coma (a.k.a. pseudocoma)
- Catatonia
- Malingering
history
It may be impossible to obtain any information regarding the history. If available, the following are notable:
- Prior medical & neurological history.
- Outpatient medication list and any recent medication changes.
- Preceding symptoms (e.g., confusion, headache, abnormal movements, weakness, depression).
- When was the patient last known to be normal?
- History of substance use?
coma neuro exam
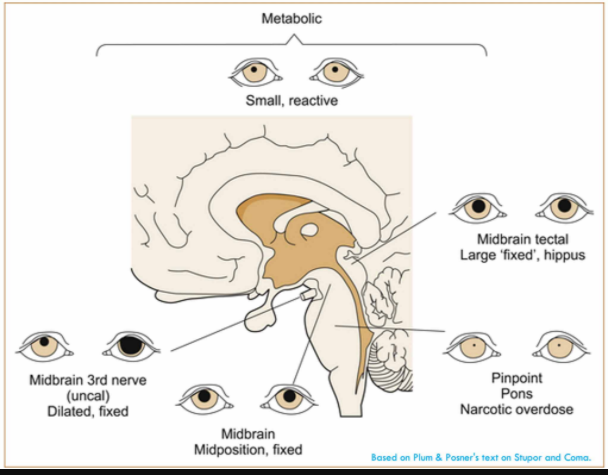
common pupillary abnormalities
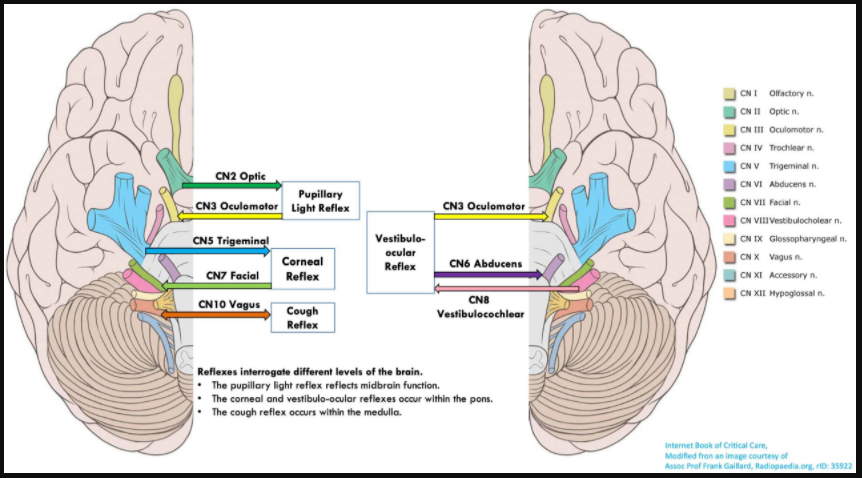
For the complete and detailed explanation of all of that follows, please click on Dr. Farkas sections:
- How to examine:
- Apply painful stimuli to four extremities and bilateral face (either supraorbital ridge or temporomandibular joints).
- Observe for motor response (e.g., purposeful avoidance of the painful stimuli, a “localizing” response to pain) as well as nonfocal grimacing. For example, grimacing without the ability to withdraw suggests an intact sensory response, but the presence of motor paralysis.
- Asymmetric responses suggest a focal lesion.
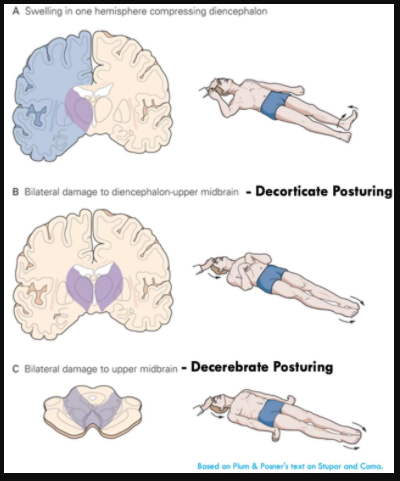
- Decorticate posturing is loosely associated with damage at the level of the thalamus.
- Decerebrate posturing is loosely associated with damage at the level of the midbrain. This is usually associated with downward herniation or compression of the brainstem by posterior fossa lesions. However, occasionally toxic/metabolic etiologies may also cause decerebrate posturing (e.g., hepatic encephalopathy).
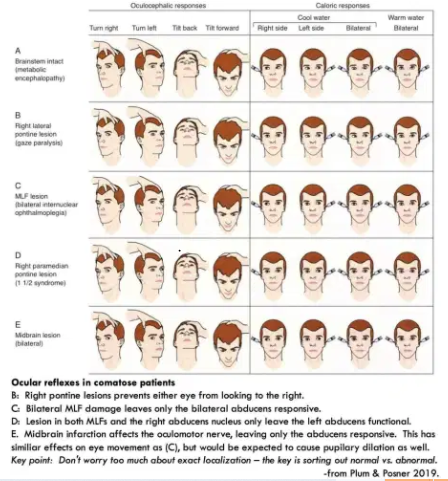
common coma syndromes
bilateral hemispheric dysfunction (e.g., most toxic/metabolic comas)
- The key finding is that brainstem reflexes are usually intact. However, reflexes may be lost in very deep toxic comas (e.g., barbiturate or baclofen overdose).
- Intact vestibulo-ocular reflexes.
- Intact pupillary and corneal reflexes.
- Spontaneous eye movements can occur (e.g., roving conjugate gaze, dipping with slow downgaze followed by rapid upgaze, or ping-pong gaze back and forth).(28187795)
- Upward or downward eye deviation can occur.
- Adventitious limb movements may be seen. If present, multifocal myoclonus, asterixis, or tremor support a metabolic etiology.(28187795) Any motor signs are usually symmetric.
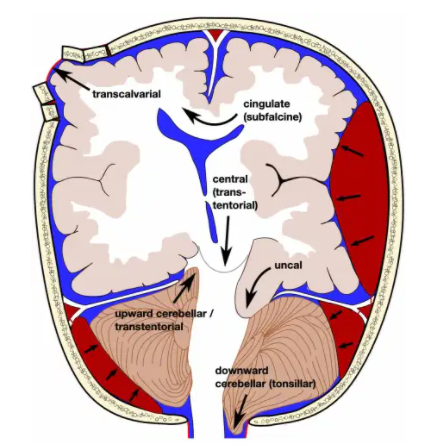
uncal herniation
- Ipsilateral blown pupil:
- Initially, the pupil is simply dilated.
- With progression, oculomotor paralysis occurs (causing the eye to be fixed in a down-and-out orientation).
- Contralateral hemiparesis due to compression of the cerebral pedicle
- Ipsilateral weakness can occur if lateral displacement compresses the opposite cerebral peduncle (a “false localizing sign”).
- Hemiparesis may be accompanied by a positive Babinski’s sign.
- If untreated, this may eventually compress the midbrain (e.g., causing bilateral fixed & dilated pupils, with decorticate or decerebrate posturing).
downward central herniation (a.k.a. downward transtentorial herniation)
- Miotic (small) pupils are initially a prominent sign.
- ⚠️ Initially, this may resemble an intoxication causing small pupils (e.g., cholinergic agonists, opioids, clonidine, ACE-inhibitors). There may initially be conjugate roving eye movements, simulating a toxic/metabolic coma.
- Abnormal motor responses (e.g., posturing) may be an early clue to a structural etiology of the coma.
- With progression of herniation:
- Midbrain dysfunction emerges: pupils may become fixed & mid-position. Vestibulo-ocular reflexes become abnormal.
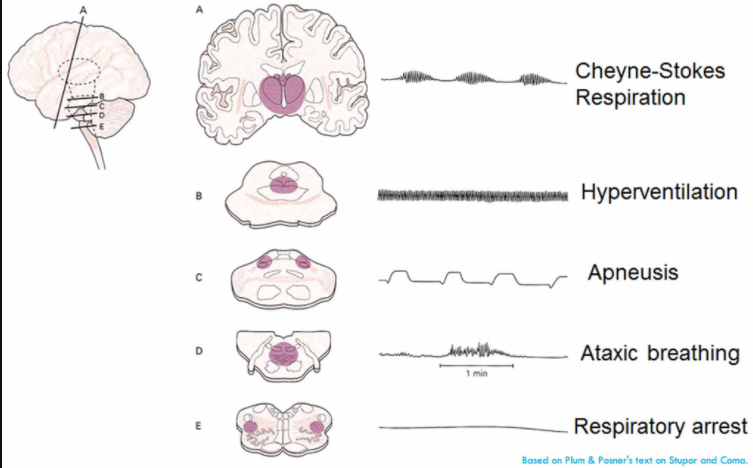
- Pathological breathing patterns may emerge (including Cheyne-Stokes breathing, irregular ataxic breathing, or neurogenic hyperventilation).
- Decorticate and later decerebrate posturing occur, with bilateral extensor Babinski reflexes.
brainstem displacement from a cerebellar mass
- Cranial nerves:
- Pupillary reflexes are often intact (since these are located in the midbrain, which is above the level of compression).
- Absent corneal reflexes and abnormal vestibulo-ocular reflexes are often seen. Skew deviation may occur (one eye looks up, the other looks down).
- Ocular bobbing can occur, or nystagmus that may be direction-changing or vertical.(28187795)
- Extensor or flexor posturing can occur.
tests & investigations
labs
- Basic labs:
- Electrolytes, including Ca/Mg/Phos.
- CBC with differential.
- Coagulation studies.
- Liver function tests, including ammonia.
- Lactate.
- Thyroid Stimulating Hormone (TSH).
- Urinalysis.
- VBG or ABG, if hypercapnia is suspected and the patient isn’t intubated.
- Toxicologic labs, depending on clinical context. For example:
- Carboxyhemoglobin level (may be obtained with venous blood).
- Salicylate & acetaminophen levels.
- Ethanol level.
- Urine toxicology screen.
- Blood cultures (if sepsis or meningitis is suspected).
- Creatinine kinase, if the patient is found down with possible rhabdomyolysis.
- Pregnancy test, if relevant.
CT scan
- (1) Most patients will receive a noncontrast head CT to exclude intracranial hemorrhage or other space-occupying lesions.
- (2) CT angiogram (CTA) and CT perfusion:
- Should be considered if there is suspicion for an acute ischemic stroke (e.g., abnormal brainstem findings on exam suggestive of basilar artery occlusion).
- (3) CT venogram (CTV):
- Thrombosis of the straight sinus may cause thalamic dysfunction, leading to coma.
- CT venogram should be considered if there is suspicion of venous sinus thrombosis.
lumbar puncture
- Indications to perform an LP:
- (1) Suspicion of meningitis or encephalitis (e.g., based on fever, leukocytosis).
- (2) Lack of any alternative explanations for the coma following review of neurologic examination, labs, and neuroimaging.
- In situations where there is low index of suspicion for meningitis or higher risk from lumbar puncture (e.g., coagulopathy), a contrast-enhanced MRI may be considered as an alternative evaluation for meningitis or encephalitis.(24977138)
- Basic CSF investigations should include the usual chemistries and cell counts, as well as PCR for both HSV and VZV. Immunocompromised patients should be tested more broadly (e.g., including cryptococcal antigen). Cytology should be obtained if leptomeningeal carcinomatosis is suspected.
- Elevated opening pressure may suggest infection (e.g., bacterial or cryptococcal meningitis), venous sinus thrombosis, acute liver failure, or leptomeningeal carcinomatosis.
- Additional fluid should be held for more sophisticated testing if needed (e.g., paraneoplastic or autoimmune antibody screens).
EEG
- EEG may be indicated if there are reasons to consider nonconvulsive status epilepticus, such as:
- Seizure history (current or prior).
- Clinical indications of possible nonconvulsive status, for example:
- Focal twitching of the hands or face, nystagmus, eye blinking, or chewing movements.
- Recurrent pupillary hippus (pupils dilating/constricting spontaneously), pupillary dilation.
- Focal neurologic findings despite a normal CT scan (e.g., gaze deviation).(28187795)
MRI
- MRI is indicated if the above workup fails to reveal a diagnosis.
- Gadolinium contrast may improve the yield for infection or malignancy, so this may be especially useful if a lumbar puncture hasn’t already been performed.(24977138)
- MR angiography (MRA) and/or MR venography (MRV) may be considered, similarly to CT angiography and CT venography (e.g., based on the index of suspicion for cerebral venous sinus thrombosis).
- If the patient isn’t already intubated, then intubation should be strongly considered prior to MRI to ensure airway protection. Additionally, intubation with deep sedation (often with propofol) may facilitate a high-quality MRI, without movement artefact.
airway management
noninvasive ventilation (e.g., BiPAP)
- This may sometimes be considered if hypercapnia is believed to be the cause of the altered mental status.
- If COPD is the cause of the hypercapnia, then BiPAP may be trialed under close supervision (more on this in the chapter on COPD).
- If hypercapnia is the result of substance intoxication or neurological disease, BiPAP is contraindicated. The management of marked hypercapnia in this context is generally intubation. However, for moderate substance intoxication, if the patient is protecting their airway and they are only moderately hypercapnic, then close observation might be adequate (without either BiPAP or intubation).
consider intubation
- Common indications for intubation in this context:
- (a) Failure to protect the airway.
- (b) Intubation may be required to accomplish diagnostic testing safely (e.g., LP, MRI).
therapies to consider
dextrose
- Glucose should be checked immediately in any patient with altered mental status.
- If hypoglycemia cannot be excluded immediately, give an ampule of D50W empirically (e.g., while awaiting the return of values from the laboratory).
thiamine
- Wernicke’s encephalopathy should be considered in patients with alcoholism, bariatric surgery, eating disorders, or malabsorption.
- When in doubt, treat empirically with 500 mg IV thiamine Q8hr (more on Wernicke’s encephalopathy here).
naloxone
- Suspect opioid intoxication primarily if the respiratory rate decreased.
- If opioid intoxication is possible, naloxone may be empirically trialed with increasing doses to a cumulative dose of ~4 mg.(26438464)
- Note that patients on chronic opioid will generally experience pain and agitation after naloxone, due to withdrawal of opioid effects. This doesn’t prove that their stupor/coma is caused solely by opioid, unless they are able to wake up and mentate normally.
- Increased agitation or pain due to naloxone implies having had exposure to opioid, but doesn’t necessarily exclude other pathology.
empiric therapy for meningitis & encephalitis
- If there is a significant concern for meningitis, empiric therapy should be given immediately (even before CT or lumbar puncture).
- A reasonable approach is generally:
- 10 mg dexamethasone, followed by ceftriaxone 2 grams IV q12hr.
- Acyclovir 10 mg/kg IV q8hr.
- The added yield of vancomycin and ampicillin here is extremely low, because most of these patients don’t actually have meningitis (and the added benefit from vancomycin and ampicillin in meningitis is minimal).
- More on empiric therapy for meningitis here.
osmotherapy & ICP management
Start here.