Here are links to and excerpts from COVID-19: a remote assessment in primary care [PubMed Abstract] [Full Text HTML] [Full Text PDF]. BMJ 2020;368:m1182 (Published 25 March 2020).
Here are excerpts:
At the time of writing, the situation is changing rapidly. This
article will be updated as new evidence emerges. National and
local protocols are likely to emerge for the topics covered in
this article and other aspects of care in covid-19.The sick patient
Patients who are very unwell, and especially those with possible
pneumonia, need to be urgently assessed either by video or in
person, depending on the clinical circumstances. The clinical
criteria for hospital admission in covid-19 pneumonia are the
same as for any other pneumonia, but in the current crisis there
may be additional restrictions.The best clinical signs to predict community acquired pneumonia in an adult are a temperature above 38°C, respiratory rate above 20 breaths/minute, and heart rate above 100 beats/minute with new confusion; low urine output is also a concerning symptom.13
Anecdotal reports from UK secondary care suggest that hypoxia is often used as a cut-off for admission. Both the World Health Organisation and a guide based on the China experience recommend a cut-off level of 93% for classifying pneumonia as severe.14 15
Current UK NHS guidance recommends hospital admission if saturation on air is below 94%.16 Additional features in children include grunting, central cyanosis, and inability to breastfeed.14 15
We recommend that, in the case of patients with a very poor
prognosis (for example, multimorbidity and other risk factors),
a “ceiling of treatment” conversation is considered.17 If the
patient is very sick and death almost inevitable whether
ventilated or not, some people may prefer to stay home and opt
for palliative management. Many such patients will already
have an advance care plan and DNACPR (do not attempt
cardiopulmonary resuscitation) flag, and in those who do not,
urgent efforts should be made to put these in place to avert
unwanted emergency intervention.What you need to know
- Most patients with covid-19 can be managed remotely with advice on symptomatic management and self isolation
- Although such consultations can be done by telephone in many cases, video provides additional visual cues and therapeutic presence
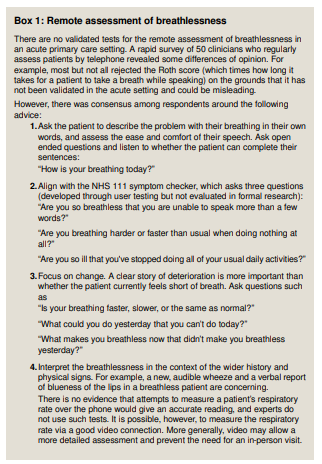
- Breathlessness is a concerning symptom, though there is currently no validated tool for assessing it remotely
- Safety-netting advice is crucial because some patients deteriorate in week 2, most commonly with pneumonia
Taking a history
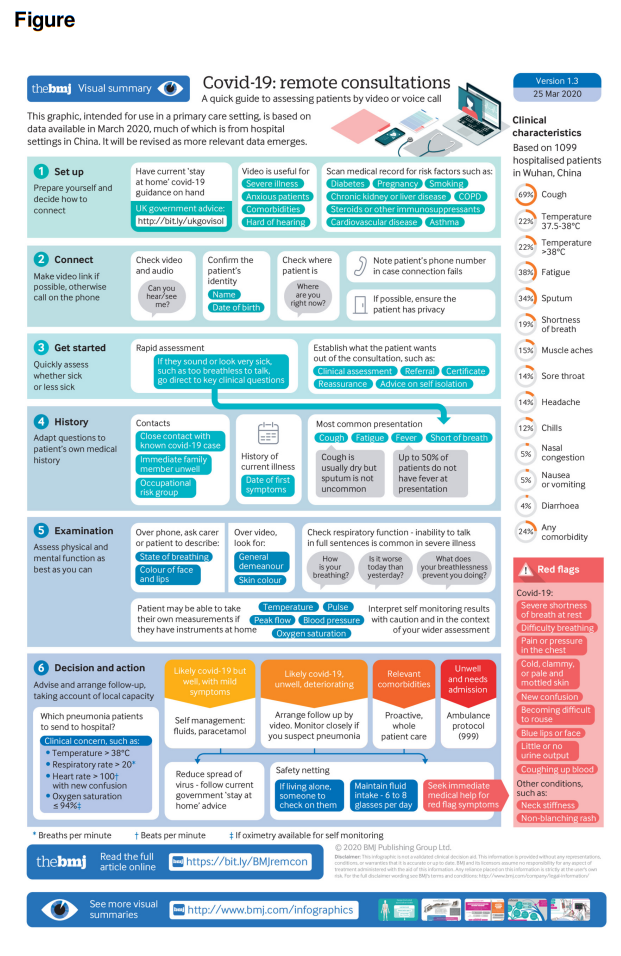
Note the approximate incidence of key symptoms and signs
listed in the infographic (right hand column), with the caveat
that this list was generated in a different population and may
not reflect your own case mix. The infographic guidance should
be used flexibly to take account of the patient’s medical history
and issues that emerge during the conversation. The vignette [in the article] describes a typical mild to moderate case of this disease; more serious cases typically develop worsening respiratory symptoms, which may indicate pneumonia. Elderly and immunocompromised patients may present atypically.Note the date of first symptom to date-stamp the onset of disease. Many but not all patients will have a thermometer at
home. Ask how high their temperature is currently, how long
the fever has lasted, and what the highest reading so far has
been. The fever in covid-19 is often but not always >38.0°C
and tends to persist beyond five days. Note that up to half of all
patients with covid-19 have no fever at initial presentation.Ask about a history of contact with a case of covid-19
(laboratory confirmed or clinically suspected), especially one
who had been closer than 1 metre for 30 minutes or more. The incubation period for covid-19 is 2-14 days, on average 5-6
days.Features that generally indicate a condition other than covid-19
include nasal congestion (present in only 5% of cases),
conjunctival congestion (1%), and other allergic symptoms such
as itchy eyes. A preliminary report suggests that, although
conjunctival involvement is rare in covid-19, it is a poor
prognostic sign if present.9Red flags
Red flag symptoms which indicate that the patient needs urgent
assessment (either in person or by a good video link, depending
on the clinical circumstances) include severe breathlessness or
difficulty breathing, pain or pressure in the chest, blue lips or
face, and a story suggestive of shock (such as cold and clammy
with mottled skin, new confusion, becoming difficult to rouse,
or significantly reduced urine output). Haemoptysis occurs in
about 1% of covid-19 patients and seems to be a poor prognostic
symptom.
Here is a link to other BMJ infographic