In this post I link to and excerpt from Diagnosis Of Peripheral Neuropathy [Full Text HTML] [Download Full Text PDF]. Neurol. Res. Pract. 2, 20 (2020). https://doi.org/10.1186/s42466-020-00064-2
Here are excerpts:
Abstract
Introduction: Peripheral neuropathy represents a spectrum of diseases with different etiologies. The most common causes are diabetes, exposure to toxic substances including alcohol and chemotherapeutics, immune-mediated conditions, and gene mutations. A thorough workup including clinical history and examination, nerve conduction studies, and comprehensive laboratory tests is warranted to identify treatable causes.
First steps: The variability of symptoms allows distinguishing characteristic clinical phenotypes of peripheral neuropathy that should be recognized in order to stratify the diagnostic workup accordingly. Nerve conduction studies are essential to determine the phenotype (axonal versus demyelinating) and severity. Laboratory tests, including genetic testing, CSF examination, nerve imaging, and nerve biopsy, represent additional clinical tests that can be useful in specific clinical
scenarios.Comments: We propose a flow chart based on five common basic clinical patterns of peripheral neuropathy. Based on these five clinical phenotypes, we suggest differential diagnostic pathways in order to establish the underlying cause.
Conclusions: The recognition of characteristic clinical phenotypes combined with nerve conduction studies allows pursuing subsequent diagnostic pathways that incorporate nerve conduction studies and additional diagnostic tests. This two-tiered approach promises higher yield and better cost-effectiveness in the diagnostic workup in patients with peripheral neuropathy.
Keywords: Peripheral neuropathy, Diagnosis, EMG, Nerve conduction studies, Hereditary amyloid transthyretin (ATTRv)
amyloidosis, CIDP, Diabetic, UltrasoundIntroduction
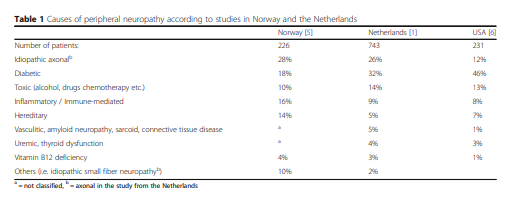
Hospital data-based epidemiological studies provide (often differing) lists of most frequent causes of peripheral neuropathy in Western countries (Table 1).
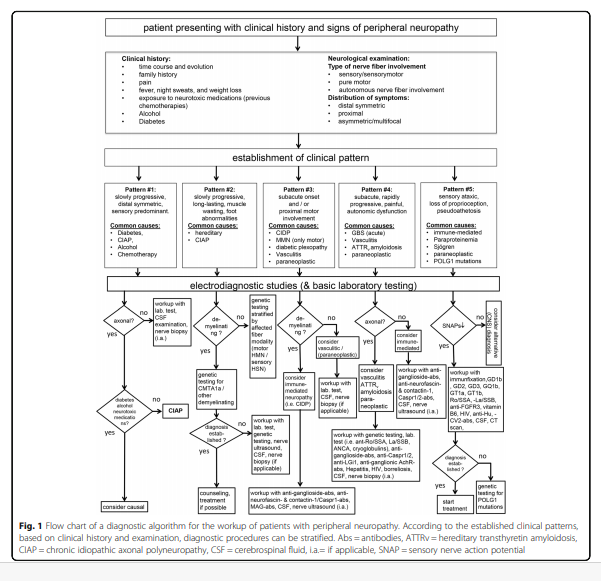
By focusing on the initial steps of the diagnostic workup, this standard operating procedure provides a practical guideline including clinical and additional diagnostic parameters that help to identify the underlying cause of peripheral neuropathy. Figure 1 provides a flow chart of this diagnostic workup.
First Steps
Recognizing specific clinical patterns is essential to stratify the diagnostic workup in a patient who presents with
signs and symptoms of peripheral neuropathy. This
workup should include a detailed history and a thorough
clinical examination. In our flow chart, we propose five
different clinical patterns:#1. Slowly progressive, distal symmetric, predominantly
sensory neuropathy: This most common peripheral
neuropathy subtype is often caused by a metabolic
condition (diabetes), chronic alcohol consumption, or
neurotoxic drugs (chemotherapy). These patients only
need limited diagnostic testing unless atypical
neuropathy features are present. Exclusion of these
causes may lead to the diagnosis of chronic idiopathic
axonal neuropathy (CIAP), which usually has a benign
course.#2. Slowly progressive, long-standing neuropathy with
muscle wasting and foot abnormalities: Motor predominant, onset in child-, or adulthood, these patients may be less frequent compared to the other subtypes. Diagnostic workup should be prioritized towards genetic
testing.#3. Neuropathy with subacute onset and/or proximal
involvement: These patients present with clinical
features suggestive of an acquired immune-mediated
condition. Extensive diagnostic workup, including antibody testing, etc. may be required.#4. Neuropathy with subacute or rapidly progressive
disease course, multifocal symptoms, neuropathic pain,
and autonomic dysfunction: Potentially caused by
vasculitis, amyloidosis, or as paraneoplastic syndrome.
Patients with this subtype should undergo detailed
diagnostic workup.#5. Sensory ataxic neuropathy: Clinical correlates of
sensory neuronopathy or Denny-Brown’s syndrome.
Patients present with loss of proprioception and vibration sense and may display pseudoathetosis, with relative preservation of muscle strength. Underlying causes
that should be explored include autoimmune disorders
(i.e., Sjögren), paraneoplastic syndromes, and mitochondrial disorders.These five subtypes should neither be taken as exclusive nor absolute since overlap of these patterns is not uncommon. For instance, some patients with a hereditary neuropathy (i.e., ATTRv amyloidosis) present with a rapidly progressive disease course, and are often misdiagnosed as CIDP. On the other hand, also CIDP patients occasionally present with a slowly progressive disease course.
Clinical History
Start review here.