In this post I link to and excerpt from Management of Asymptomatic Patients With Positive Coronary Artery Calcium Scans [PubMed Abstract] [Full Text HTML] [Full Text PDF]. J Endocr Soc. 2017 Jun 1;1(6):588-599.
Here are the excerpts:
The coronary artery calcium (CAC) scan has become popular for individuals at risk for atherosclerotic cardiovascular disease. Indeed, CAC testing is increasingly being promoted to the public as a means of self-assessment of cardiovascular risk. There are several reasons for the widespread use of the coronary calcium scan, including its relatively low cost ($50 to $200 in most cities), its excellent predictive value for atherosclerotic cardiovascular disease (ASCVD) and mortality [1, 2], the noninvasive nature of the test, the low-dose radiation exposure
(equivalent radiation to living in Denver for 3 months), and the fact that a physician’s prescription is usually not required. The number of asymptomatic individuals in the high and intermediate risk categories in the United States is large and includes all diabetic patients and individuals with sufficient Framingham risk factors and/or genetic causes of hyperlipidemia.Decisions facing clinicians after the report of a positive coronary calcium scan in asymptomatic patients are (1) which medical therapy and lifestyle modifications to recommend, (2) how aggressively to reduce plasma low-density lipoprotein cholesterol (LDL-C), and (3) whether stress testing and/or referral to a cardiologist is indicated.
This review discusses the pros and cons of these choices and makes recommendations based on the current medical literature. These recommendations apply only to asymptomatic patients without clinical evidence of heart disease and are primary prevention strategies.
In asymptomatic patients with no report of angina but a positive calcium scan, one possibility is that the physician will
order an exercise treadmill test. Excluding false-positive results (e.g., induced by spasm of a coronary artery), a positive result indicates an obstruction of a coronary artery by at least 50%.What is the next best step?
The choice is between coronary angiography with the intention to place a stent at the site of a constriction or to rapidly initiate aggressive medical therapy to reverse the atherosclerosis and the obstruction. During the reversal period, collateral channels may develop, increasing blood flow around the obstruction. Because long term follow-up (.10 years) data from patients with stable angina demonstrate that intensive medical therapy is as beneficial as placement of a stent (which is more invasive and costly), there is minimal reason to order an initial stress test in patients with stable angina [4, 5].
Although randomized clinical trials evaluating the treatment of patients on the basis of their CAC score have not been done, extensive epidemiological and observational data are compelling and deserve serious consideration to guide physicians in making correct choices to recommend to their patients. Although the Multi-Ethnic Study of Atherosclerosis (MESA) clinical trial is the most well-described study [6], other investigators have also published their observations in populations that have received coronary calcium scores. For example, Arad et al. [7] studied 1177 high-risk, asymptomatic, middle-aged adult subjects for 3.6 years. The mean coronary artery calcium score was 764 among subjects with events, compared with a mean score of 135 among those without events. They conclude that “in asymptomatic adults, EBCT (coronary calcium) predicts coronary death and non-fatal MI.”
Shaw et al. [14] studied 9715 asymptomatic individuals with a median follow-up of 14.6 years. They concluded that “the extent of CAC accurately predicts 15 year mortality in a large cohort of asymptomatic patients.”
Tota-Maharaj et al. [2] studied the predictive value of calcium scoring in both young and elderly individuals. They conclude that “the value of CAC for predicting mortality extends to both elderly patients and those less than 45 years old. Elderly persons with no CAC have a lower mortality rate than younger persons with high CAC.”
1. Risk Factor Assessment and CAC Scoring
Prior to the availability of calcium scoring, combining cardiovascular risk factors was (and remains) a popular approach to determining an individual’s overall risk of future cardiovascular events.
There are several approaches that combine several risk categories to attain an overall risk score for an individual patient (e.g., Framingham, American Heart Association, Reynolds, and MESA). One of the most popular is the Framingham Risk Score, in which several risk categories are entered into an online risk calculator and a 10-year cardiovascular risk score is generated [15]. The main differences between the various risk scores available on the internet are the specific risk categories entered and the weights given to each
category of risk. In addition, these risk scores have each undergone several revisions in attempts to improve their prognostic accuracy.The major difficulty of using all risk scores is the fact that the information entered into the risk score database reflects only one point in time, making it difficult to predict the risk in an individual whose cardiovascular risks may have changed in the past [16]. In addition, the model used to generate the risk predictions are usually based on one specific population. For example, the Framingham Risk Score is based on the white population in Framingham, MA, and may not be applicable to other racial groups.
The score assigned to a CAC scan summarizes the degree and extent of calcium contained in the four major coronary arteries and thus defines the magnitude of cardiac atherosclerosis
present. The most commonly used scoring system is the Agatston score [17], which involves identifying “regions of interest” that contain calcium within coronary arteries and determining the area of all lesions > 1 mm2 in total area as well as the maximum calcific density for all lesions > 130 Hounsfield Units. In spite of its limitations, the Agatston score has a long
track record of proven utility in predicting new ASCVD events and remains the most widely used CAC scoring method for clinical application [18].Although coronary angiography has often been considered the “gold standard” approach to defining the severity of atherosclerosis, recent studies have shown that CAC scores are better predictors of future cardiovascular events in asymptomatic individuals [19–22].
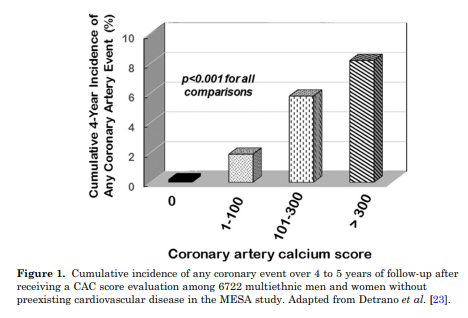
For example, in the MESA study, 6722 men and women were followed for a median of 3.8 years (Fig. 1) [23].
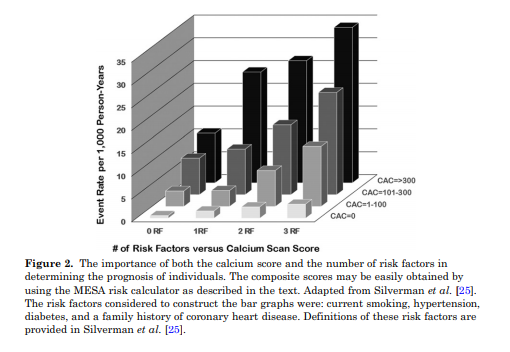
As shown in Fig. 2, when combined with traditional risk factors, the baseline CAC score predicted future cardiovascular events with improved accuracy.
When the Framingham Risk score and the CAC score are combined, an improved prognostic outcome can be calculated [1]. Easy access to this improved, validated tool for cardiovascular event prediction is available at https://www.mesa-nhlbi.org/MESACHDRisk/MesaRiskScore/
RiskScore.aspx [24].The presence of calcium in coronary arteries is very strong evidence of the presence of atherosclerotic plaque [19]. The calcium should be considered a sign of atheroma presence and not necessarily a threat for future cardiovascular events. In fact, the majority of infarction-associated arterial thromboses are due to rupture of noncalcified, nonobstructive plaques [26].
2. Stress Testing
Stress testing is often recommended to exclude potentially dangerous coronary artery disease. This approach involves stressing the cardiovascular system either with standardized
exercise or stimulating the cardiovascular system with medication. The primary purpose is to identify coronary artery obstructive lesions with greater than 50% luminal obstruction.
However, stress testing in asymptomatic individuals has low sensitivity and specificity (45% to 60%) [27]. The cost of the test can range between $300 and $700 depending on the institution and whether radioactive isotopes are used. Of note is that the risk to benefit ratio for adverse events increases in low-risk individuals [27].A recent review of coronary angiography recommends caution in the use of this test because (1) the resolution of coronary angiography is low; (2) the obtained images are two dimensional, making it difficult to define the shape of the vessel; and (3) the assessment of obstruction does not include the presence of previously developed collateral vessels, which may provide adequate blood flow past the obstruction [28].
According to the US Preventive Services Task Force: “The primary tangible harm of screening exercise tolerance
testing is the potential for medical complications related to cardiac catheterization done to further evaluate a positive result. Coronary angiography is generally considered a safe
procedure. Of all persons undergoing outpatient coronary angiography, however, an estimated 0.08% will die as a result of the procedure and 1.8% will experience a complication.
Complications of coronary angiography include myocardial infarction, stroke, arrhythmia, dissection of the aorta and coronary artery, retroperitoneal bleeding, femoral artery
aneurysm, renal dysfunction, and systemic infection” [29]. In addition, the charges for this test are between $5000 and $10,000 at most locations, and the patient’s copay for the
procedure may approach 50% [30].The greatest objection to stress testing and coronary angiography is the fact that the identification of an obstructive lesion does not usually identify future causative sites of myocardial infarctions. Because myocardial infarctions almost always result from unstable atherosclerotic plaques that rupture into the coronary artery lumen, coronary angiography
identification of an obstructive lesion does not usually identify alternative causative sites of future myocardial infarctions [26]. Unstable plaques may be far removed from the lumen narrowing lesions observed during coronary angiography.Thus, in asymptomatic individuals who have no anginal symptoms during their normal daily activities, the benefit from
ordering stress testing or coronary angiography is questionable. For the above reasons, stress testing in asymptomatic individuals has not been shown to reduce future cardiovascular events [29]. Stress testing guidelines generally discourage using this approach in asymptomatic individuals.3. Reversibility of Atherosclerosis
New information concerning the pathogenesis of atherosclerosis has become available during the last decade [31]. Both hyperlipidemia and inflammation play critical roles with other
cardiovascular risk factors, such as hypertension and diabetes, increasing cardiovascular risk [32].On the positive side, there is also ample evidence that atherosclerosis is a reversible disease. Several controlled trials have demonstrated that reversibility occurs at an LDL-C of
approximately 65 mg/dL, assuming other risk factors are also addressed [34–39].Statins, which are the mainstay of antiatherosclerosis therapy, have both LDL-C lowering and antiinflammatory activity [40]. These beneficial effects of statin therapy on atherosclerotic plaque composition can be observed within 1 month of starting statin therapy and are consistent with converting an unstable plaque to a stable plaque [41]. These observations provide a strong impetus for physicians to aggressively address risk factors, contributing to an initial positive calcium score.
4. Aggressive Medical Therapy
Most major professional organizations recommend an LDL-C < 70 mg/dL for patients at increased ASCVD risk. The LDL-C principle, which was recently reviewed [42], states that the lower the LDL-C concentration, the lower the incidence of a cardiovascular atherosclerotic events (there is no lower threshold for a beneficial effect). This principle suggests that LDL-C level < 70 mg/dL should be the goal for everyone with an elevated risk for cardiovascular disease and that an even lower LDL-C level should be the goal for individuals with multiple risk factors [42].
Achieving an LDL-C goal of < 70 mg/dL is possible in almost all individuals without a genetic cause of severe hyperlipidemia. Moreover, no unexpected side effects have been observed at LDL-C levels < 50 mg/dL [43]. Because most individuals were born with an LDL-C of between 50 and 70 mg/dL, these levels should not be considered abnormal [44]. In addition, the normal LDL-C range is 50 to 70 mg/dL for native hunter-gatherers, free-living primates, and other wild mammals (none of which develop atherosclerosis) [45]. Because all cells in the body have the capacity to synthesize cholesterol, additional cholesterol from circulating LDLC is not required in adults for health, and the recent availability of high-potency statins,ezetimibe, and PCSK9 inhibitors make the goal of > 70 mg/dL practical [46, 47].
5. Medical Therapy vs Percutaneous Intervention
[There are no clinical trials comparing medical therapy alone versus percutaneous coronary interventions (PCI) in asymptomatic patients with a positive calcium score.]
[But] that compare medical therapy vs PCI plus medical therapy in individuals with stable angina. These individuals usually do not have symptoms of angina at rest, although they may have
angina with exercise. The conclusion of a meta-analysis examining these studies concluded no benefit of PCI beyond that achieved with optimal medical treatment except relief of angina,
particularly for single-vessel disease [4, 48, 49].In addition, the longest observational study available (15 years) demonstrated no difference in mortality between PCI and medical therapy in these patients [5].
Furthermore, what formerly was considered “optimal medical
therapy” no longer meets current treatment guidelines because improved medications to treat atherosclerosis are now available [42].6. Antihyperlipidemic Therapy