In this post I link to CORE IM’s September 30, 2020 COVID Management Update podcast and show notes.
Here are excerpts:
Time Stamps
- 04:16 Supportive Care
- 07:48 Step-up approach to oxygenation
- 13:44 Data Points
- 15:30 Clots
- 19:13 Steroid use
Show Notes
Part 1: Supportive Care
- Care for COVID patients in the ICU is not different than care for other critically ill patients. It depends on data collection/interpretation and regimented decision-making
- Supportive care seems basic, but is one of the most important parts of caring for COVID patients
- Supportive care falls into a few different buckets – early mobilization, removing unnecessary lines, lung protective ventilation
- The most important thing is to pay attention to their vital signs and think about basic needs of our patients – develop your differential diagnosis for things like hypotension, hypoxia, and tachycardia so that you can appropriately evaluate and treat your patients
Part 2a: Oxygenation
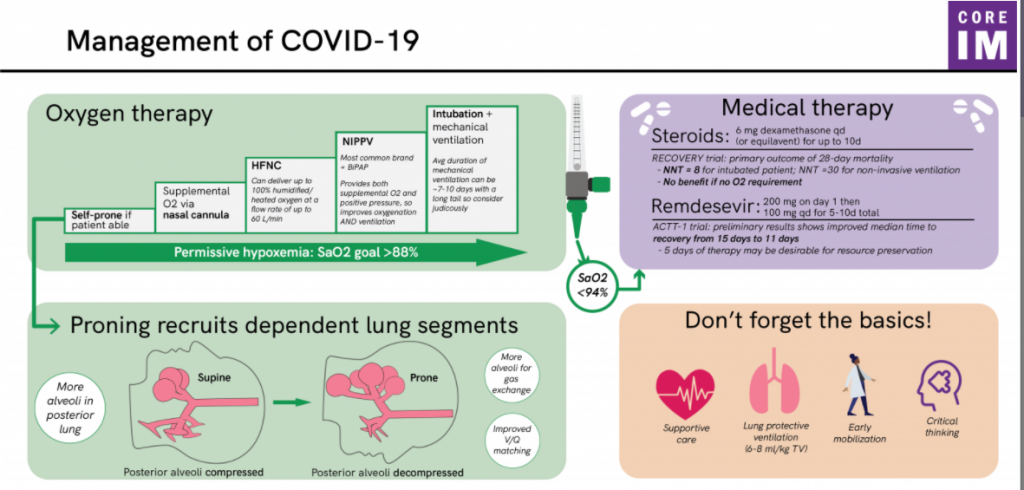
- Think in terms of a step-up approach to oxygenation – self proning, supplemental oxygen, noninvasive positive pressure, and mechanical ventilation
- Self proning benefits patients in a few ways – decreasing V/Q mismatch, recruiting dependent lung segments, better drainage of secretions, improved hemodynamics. Most importantly, patients feel better!
- Supplemental oxygen means everything from nasal cannula to face mask
- High flow nasal cannula is mostly supplemental O2 with a small amount of positive pressure
- Noninvasive positive pressure ventilation – usually referred to by the trade name of BiPAP – can be used with reasonable infection control. We were worried about this at the beginning of the pandemic, but can be done safely with precautions taken
- It’s ok to tolerate permissive hypoxemia if you can stave off intubating patients
- Intubation doesn’t just mean mechanical ventilation – it also means sedation, immobilization, infection risk
- The duration of mechanical ventilation can approach two weeks with a long tail
Part 2b: Labs
- Trending daily CRP, ESR, D-dimer, troponin, LDH, etc probably doesn’t provide much useful information
- If you don’t know what you’re going to do with a test result – or don’t know what you’re looking for in the first place – it may be better not to order it
Part 3: Anticoagulation
- Anticoagulation has been a source of controversy throughout the pandemic
- There is observational data suggesting mortality benefit from full-dose anticoagulation in hospitalized patients
- Remember that observational data needs to be interpreted with caution – it is generally considered hypothesis-generating and not proof.
- DVT prophylaxis is clearly appropriate
- Clinical vigilance for clots is also appropriate – think about DVT when a patient has unilateral lower extremity swelling or a PE with new tachycardia and hypoxia
- Critically ill patients can develop clots regardless of what makes them critically ill. It’s not clear that there’s something special about COVID that makes patients more hypercoagulable than other critically ill patients
Part 4: Medications
- RECOVERY trial demonstrated a clear mortality benefit from dexamethasone in severe COVID, particularly in ventilated patients
- Dexamethasone use for up to 10 days resulted in a lower 28-day mortality
- Benefit of steroids appears consistent across different trials and in a meta-analysis
- Remdesivir – a viral RNA polymerase inhibitor – seems to reduce time to recovery
- Remdesivir is best given early in course and a 5 day treatment duration is probably sufficient.
- Hydroxychloroquine does not have a role in treating COVID.
- IL-6 inhibitors, convalescent plasma, and other immunomodulators feel exciting, but we just don’t have any clear clinical benefit. Role for these treatments outside of clinical trials should be limited
- It is ok to continue ACE inhibitors or angiotensin receptor blockers. Indications for these medications don’t change just because someone has COVID and there is no need to stop them related to COVID risk.
Part 5: Recovery
- No one leaves the ICU the same as they entered. Long term effects in ICU survivors are common
- Post intensive care syndrome (PICS) can lead to significant long term morbidity
- Data on post COVID syndrome are heterogeneous and limited conclusions can be drawn, but clinicians should be aware that COVID patients may still be suffering after recovery from acute infection and hospital discharge