For detailed information on the treatment of STDs, please see the CDC’s Sexually Transmitted Diseases Treatment Guidelines, 2015 [Link is to the complete PDF]. From the Morbidity and Mortality Weekly Report, June 5, 2015.
In this post, I link to and excerpt from the CDC’s “Recommendations for Providing Quality Sexually Transmitted Diseases Clinical Services, 2020” [Link is to the PDF]. From Morbidity and Mortality Weekly Report, Jan 3, 2020.
Here are excerpts:
Rationale
With increasing rates of most STDs in recent years (2),
all providers have a role in the assessment of STD risk and
management of infections. STD clinics will continue to be
locations of expert care and are increasingly recognized as
venues to provide HIV preexposure prophylaxis (PrEP) to
prevent incident HIV infections (16). Providers in primary
care offices, family planning clinics, and community-based
clinics will continue to diagnose STDs among asymptomatic
patients who are especially at risk for STDs. Recommendations
for operationalizing STD care in health care settings are needed
because provision of STD services varies. This report (hereafter
referred to as STD QCS) describes what constitutes quality STD
clinical services in primary care and STD specialty care settings.CDC’s Sexually Transmitted Diseases Treatment Guidelines,
2015 [Link is to the PDF] (hereafter referred to as the STD Guidelines) providesclinical guidance to physicians and other health care providers on the prevention, diagnosis, and treatment of STDs in the United States (17). The recommendations in STD QCS are intended to complement the STD Guidelines; as such, the STD Guidelines has not been modified. Rather, this report provides guidance on clinical operations and the types of services that should be available for STD care.STD QCS describes optimal services for the provision of quality STD-related clinical care by setting, including services that should be available at the time of the patient visit. Availability of same-day, on-site tests can reduce diagnostic delays and decrease excessive and costly presumptive treatment (18). On-site medications for STDs can minimize the duration of infectiousness and reduce STD transmission, decrease the cost of staff needed to follow up on positive tests and verify treatment, and lessen complications in the interval between testing and return visits for therapy
Scope and Audience
The recommendations in STD QCS apply to private and
public providers of STD clinical services, including those in
primary care settings (e.g., internal medicine, family medicine,
or obstetrics-gynecology private offices; school-based health or
community health centers; correctional health care settings;
or HIV-care clinics) as well as those in sites dedicated to STD
service delivery (e.g., STD or sexual health clinics).STD QCS recommendations address the following questions:
- What STD-related clinical services should be available
to persons who have or are at risk for STDs, including
asymptomatic persons, in primary care settings?- What STD-related clinical services should be available
to persons who have or are at risk for STDs in STD
specialty care settings?- Which STD-related conditions should be managed
through consultation with or referral to a specialist?Recommendations
STD QCS recommendations are outlined in the following
eight sections: 1) sexual history and physical examination,
2) prevention, 3) screening, 4) partner services, 5) evaluation of
STD-related conditions, 6) laboratory, 7) treatment, and 8) referral to a specialist for complex STD or STD-related conditions.Boxes 1–7 include the recommendations for basic STD care and
specialized STD care. Citations of official guidelines and studies
that support these recommendations accompany each section
of recommendations.Box 8 includes a list of complex STD or STD-related conditions that primary care and STD specialty care settings should refer to a specialist.
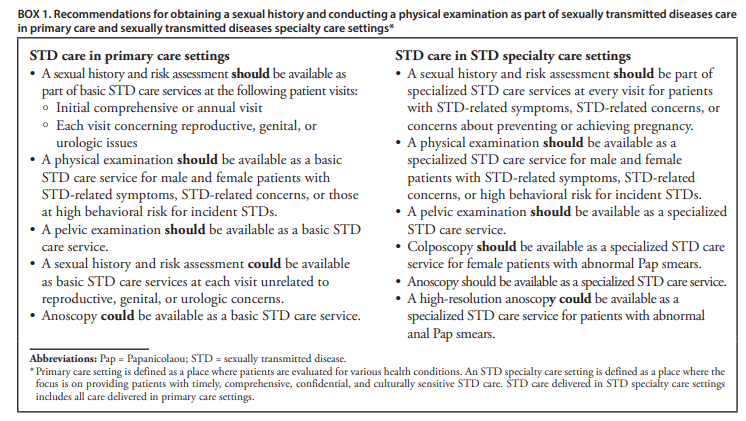
Sexual History and Physical Examination
A sexual history and risk assessment are foundational to providing quality STD care services (17,70,71). A complete
sexual history includes inquiring about the five Ps (i.e., partners,
practices, protection, past history of STDs, and prevention of
pregnancy) (17). A Guide to Taking a Sexual History is available
(https://www.cdc.gov/std/treatment/sexualhistory.pdf).A physical examination for STDs includes inspection
of the skin, pharynx, lymph nodes, anogenital area, and
neurologic system. The examination can provide useful
information among males and females with STD-related
symptoms (17,70–73). A physical examination allows health
care providers the opportunity to identify the presence of any
signs of STDs of which a patient might or might not be aware.An anogenital examination for females includes a pelvic
examination with three elements: 1) inspection of the
external genitalia, urethral meatus, vaginal introitus, and
perianal region; 2) speculum examination of the vagina and
cervix; and 3) bimanual examination of the uterus, cervix,
and adnexa (72)An anogenital examination for males includes an external
genital examination and inspection of the penis, scrotum,
scrotal contents, and perianal region (74). An anoscopy can
assist with the visualization of the anal canal among patients
with rectal symptoms or history of receptive anal intercourse.Sexual history and physical examination recommendations are
summarized (Box 1).
Prevention
Services for preventing STDs and related conditions,
including HIV, consist of eight strategies. These are 1) condom
provision (17,70,75); 2) hepatitis A vaccination (17,76);
3) hepatitis B vaccination (17,77); 4) human papillomavirus
(HPV) vaccination (78,79); 5) emergency contraceptive
pills (17,80,81); 6) STD/HIV prevention counseling (brief,
moderate intensity, or high intensity) (17,82–84); 7) PrEP
for HIV prevention risk assessment, education, counseling,
provision, and linking or referral, or both (85); and
8) nonoccupational postexposure prophylaxis (nPEP) of HIV
risk assessment, education, counseling, provision, and linking
or referral, or both, to HIV care (86).Guidance for clinical providers on contraceptive services are outlined in Providing Quality Family Planning Services: Recommendations of CDC and the U.S. Office of Population Affairs (87)
Guidance for clinical providers on linkage to and retention in HIV medical care is outlined in the Recommendations for HIV Prevention with Adults and Adolescents with HIV in the United States, 2014 Summary for Clinical Providers (88).
Prevention recommendations are outlined (Box 2).
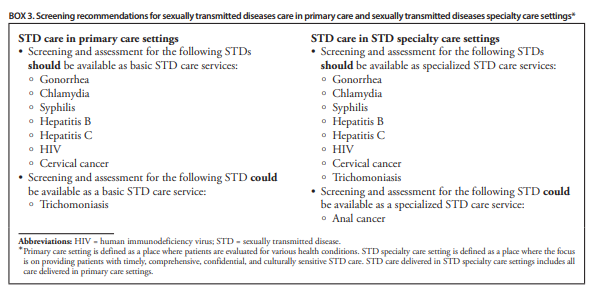
Screening
Screening for asymptomatic STDs is important for early
detection and prevention of STDs. Because many STDs
are asymptomatic, testing is the only method to diagnose
these infections. The availability of screening tests are key
for identifying gonorrhea, chlamydia, syphilis, hepatitis B,
hepatitis C, HIV, trichomoniasis, and cervical and anal cancer
(17,84,89–99). Results from these screening tests can be
used to identify persons at risk for STDs (17).Data are insufficient to recommend routine anal cancer screening with anal cytology among persons with HIV infection, men who have sex with men (MSM) without HIV infection, and
the general population (17). However, some clinical centers
perform anal cytology to screen for anal cancer among high-risk populations followed by a high-resolution anoscopy for those with abnormal cytologic results. Colposcopy is a recommended tool for cervical cancer screening.Recommendations for STD screening are listed (Box 3).
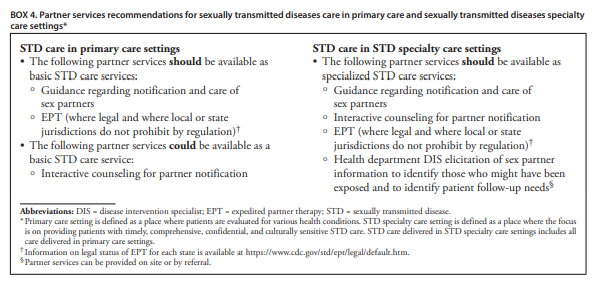
Partner Services
Treatment of sex partners prevents reinfection and is essential
to interrupting transmission of STDs. Partner services consist of various strategies with differing levels of time and effort to enable persons who are exposed to an STD to be identified, tested, and treated.Guidance regarding notification and care of sex partners
is described as providers giving how-to information to their
patients about the need to notify their sex partner or partners
of the exposure, the need for sex partners to seek care and
treatment even if they do not have symptoms, and where a
partner could go for STD care.Expedited Partner Therapy (EPT)* typically is recommended for sex partners of patients who have received a diagnosis of chlamydia or gonorrhea, or both, and who are unlikely to access timely care. This is a method that provides medications or prescriptions to the patient to take to a partner without the partner first being examined by a health care provider.
*See Expedited Partner Therapy from the CDC:
Expedited Partner Therapy (EPT) is the clinical practice of treating the sex partners of patients diagnosed with chlamydia or gonorrhea by providing prescriptions or medications to the patient to take to his/her partner without the health care provider first examining the partner.
CDC has concluded that EPT is a useful option to facilitate partner management, particularly for treatment of male partners of women with chlamydial infection or gonorrhea. Although ongoing evaluation will be needed to define when and how EPT can be best utilized, the evidence indicates that EPT should be available to clinicians as an option for partner treatment. EPT represents an additional strategy for partner management that does not replace other strategies such as provider-assisted referral, when available.
Partner services recommendations are outlined (Box 4).
Evaluation of STD-Related Conditions
Start here.