In this post, I link to and excerpt from The Cribsiders‘ #29: Tox Rocks! An Overview of Pediatric Toxic Ingestions with Dr. Diane Calello. JULY 14, 2021 By DR SAM MASUR.
All that follows is from the above resource.
Pediatric Poisoning Pearls
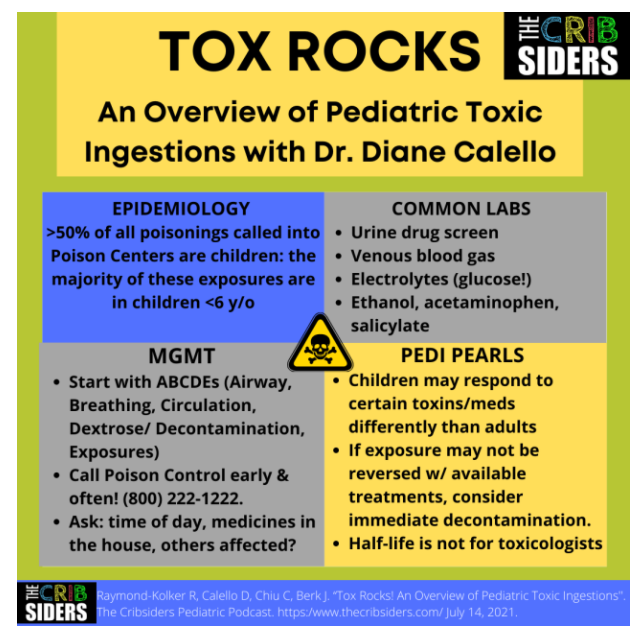
- Over half of all poisonings called into Poison Centers are children–with the majority of exposures in children under the age of 6 years old.
- In an undifferentiated ingestion–always start with your ABCDEs. Airway, Breathing, Circulation, Dextrose and Decontamination, and Exposures
- Call the Poison Control Center early and often! They are available 24/7 and are happy to support any parent, individual, or clinician. Call: (800) 222-1222.
- Children may respond to certain toxins or medications differently than adults! Be aware of the specific dangers that children face
- If any exposure may not be reversible or fixable with available treatments, this is when you should consider immediate decontamination.
- Half-life is not for toxicologists. Half-life is measured in therapeutic conditions, and it’s based on things like the function of enzymes (which get overwhelmed in overdose) or ability of the kidney to excrete it. For these reasons, knowing the half-life of a drug doesn’t help guide management in an overdose.
Epidemiology of Poison Exposures
Dr. Calello shares that over half of all the poisonings called into Poison Centers are kids (under 19 years of age). The majority of those are children under the age of 6.
Then there is a valley from 6-10 years of age where there are fewer cases. Then cases rise again in the teenage years which are more often substance use or suicidal intent which leads to poisoning.
Approach to an Undifferentiated Ingestion
Always start with your ABCDEs! D stands for Dextrose and Decontamination. [ie, Resuscitate first, if needed] You’ll never go wrong if you start with the basics. In terms of gathering a history, think of what time of day it is; if it’s a kid who didn’t wake up in the morning, they might have been exposed the night before; if the kid was last seen well about 30 minutes ago, this was a more recent exposure. Ask what medications are in the house and what health conditions other members of the household have (high blood pressure, diabetes). If the patient was found near pills or have residue on their mouth, these can be helpful clues (you can call the Poison Center to help look up a pill imprint). If anyone else in the house was affected, this suggests an environmental exposure (e.g. carbon monoxide) or siblings who got into a common toxicant. Make sure to ask when the kid last looked okay and ask if something like this has ever happened before (sometimes, inborn errors of metabolism can masquerade as toxic ingestion presentations). Ask in a nonjudgmental and private way, if anyone who lives in the house uses substances. Children who live in homes where there is a substance use disorder are at much greater risk of high mortality from poisoning.
Labs
For labs, order tests for toxidromes that you wouldn’t be able to pick up on an exam.
- You can get a urine drug screen (sometimes it is ordered because it just makes us feel better or sometimes it can be helpful in an undifferentiated ingestion), however many substances you can tell by physical exam.
- You cannot tell if a child is acidotic by exam, and so a Venous Blood Gas (VBG) is helpful to assess pH (no need to do an arterial stick).
- Electrolytes are helpful. You must always get a glucose- as many ingestions can cause low blood sugar and hypoglycemia can present as anything from an obtunded child to a focal neurologic deficit.
- An ethanol level is easy to get as well. We get in the habit of ordering an acetaminophen and aspirin level, however the likelihood of occult acetaminophen or salicylate poisoning without some history is less likely.
VAPING LIQUID
For nicotine poisoning, the best test is the clinical exam. Look for muscle fasciculations, GI symptoms, seizures. A nicotine level or a cotinine is not helpful for the short term. Vaping liquid can contain THC (tetrahydrocannabinol). Vaping associated lung injury (EVALI) is still occurring, and is seemingly linked with mostly THC-containing vapes.
When to Call the Poison Center
When shouldn’t you call the Poison Center?! Call as often and as soon as you need! Many times the Poison Center is already aware of patients seeking medical care, as parents/caregivers may have called first from home. Unlike other consultants where you may call for a specific question after a thorough workup, the Poison Center is very happy to have the provider call as cases are evolving, and walk the team through the workup and management of patients who are presenting with a concern for ingestion.
WHAT ARE POISON CENTERS? WHO WORKS THERE?
There are 55 Poison Centers across the USA. People on the other end of the phone are nurses, pharmacists, physicians, nurse practitioners, and physician assistants’ who undergo specific training in poisoning and become certified Specialists in Poison Information (SPIs). Some centers are remote, some are in person. Poison Centers operated 24/7, 365 days a year, with a relatively small staff (10-15). In addition to specialized training and expertise, SPIs have access to certain databases like Micromedex to figure out how much of a given exposure is too much and to Material and Safety Data Sheets (MSDS) to determine contents of non-food products. Behind every SPI is a toxicologist for further support in complicated cases. There is a National Poison Center Hotline at 1- 800-222-1222 which will route callers to the Poison Center you are closest to (or area code you are calling from). Many Poison Centers also have chat and text capability.
Common Ingestions
For young kids, most common calls to the Poison Center are for soap and other household items (cosmetics, cleaning products). Silica gel packs and glow sticks are responsible for a ton of calls and both are non-toxic. The preponderance of calls are non-toxic ingestions. For teenagers and adults, the most common ingestions are analgesics (acetaminophen, ibuprofen, and then opioids). The frequency of analgesic ingestions follows availability, and since acetaminophen is present in so many households, this is the most common.
Physical Exam and Toxidromes
Think of the big categories of toxidromes: Cholinergic, Anticholinergic, Opioid, Sedative Hypnotics, and Pathomimetics.
To start, ask yourself, “are they up or are they down?”
Are they sedated? Think opioids and sedative hypnotics, and cholinergics (eg pesticides with which you will also see bradycardia and bronchorrhea).
Are they revved up? Think amphetamine exposure (high blood pressure, fast heart rate) or jimson weed (dry, flushed, with huge pupils). So start by thinking, are they up or down? And then look at pupils, skin moisture, vital signs, and then pattern recognition of other findings.
- Hyperthermia (drug induced hyperthermia): can be secondary to stimulants, serotonin syndrome, neuroleptic malignant syndrome, weight loss supplements.
- Cyanosis: hypoxia, dyshemoglobinemia (such as methemoglobinemia)
- Appearance of skin, nails, teeth can be suggestive of more chronic exposures such as lead
Pediatric Population Considerations
Start here.