In this post I link to and excerpt from The Cribsiders‘ [Link is to complete episode list] #2:Go with the High Flow: Bronchiolitis with Dr. Brian Alverson
JULY 15, 2020 By JUSTIN BERK:
Summary
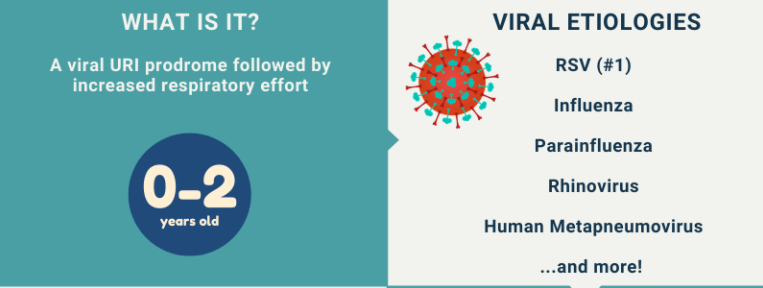
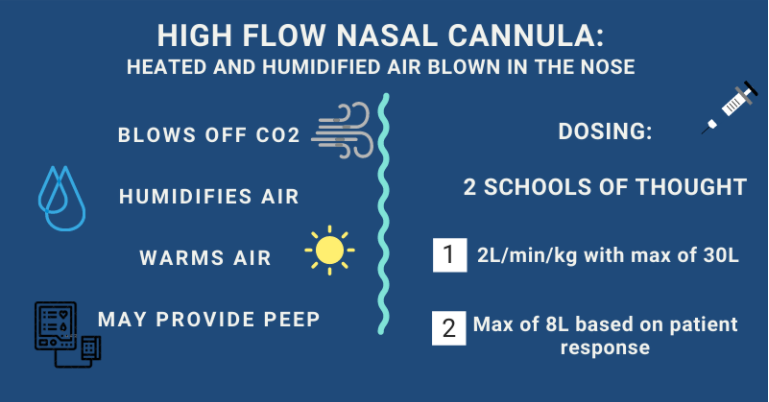
Dive into one of the most common pediatric problems, bronchiolitis, with our guest Dr. Brian Alverson, director of the Division of Hospital Medicine at Hasbro Children’s Hospital. In this episode, we review the workup of bronchiolitis, including the role of the chest x-ray, RPP, CBC, and more. We also discuss the evidence behind treatments such as albuterol, steroids, and high flow nasal cannula. Listen to hear more about this breathtaking topic.
Excerpts from the show notes:
Bronchiolitis Pearls
- Transient hypoxemia is not dangerous and is well tolerated in infants.
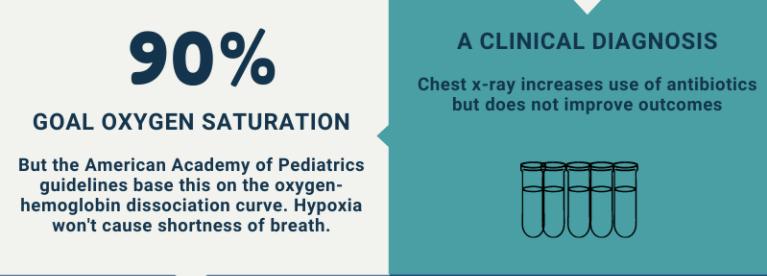
- In kids who have viral symptoms, chest x-ray increases use of antibiotics but does not improve outcomes.
- Bronchiolitis is a waxing and weaning disease.
- Less frequent superficial nasal suctioning is associated with longer hospitalizations.
- Readmission rates are associated with living closer to the hospital, young age, and low income zip code.
Approach to Diagnosis
- Bronchiolitis is a viral infection that is present in the nose and causes mucus production and then progresses to the small areas of the lungs, which makes it hard for babies to breathe.
- Expert opinion: Presume infants with a URI prodrome followed by increased respiratory effort have bronchiolitis to avoid over-testing and over-treating which can cause harm to the patient. Think broader and formulate a differential diagnosis as time passes or the child gets sicker.
Respiratory Assessment
Bronchiolitis versus bronchitis
- Bronchiolitis and bronchitis can both be caused by viruses.
- Editor’s note: Acute bronchitis involves the large airways (bronchi) compared to bronchiolitis which involves the small bronchi and bronchioles.
Respiratory Status
- Work of breathing can be assessed with retractions
- Retractions are the result of non-compliant lung due to mucus which prevents the lung from expanding and contracting normally
- Children deteriorate when work of breathing exhausts respiratory muscles.
- Expert Opinion: A patient’s respiratory status is more concerning than mild hypoxemia. Practitioner gestalt of the patient, beyond the work of breathing, often plays a role in noticing when a child is in distress.
The Febrile Bronchiolitic
To Tap or Not to Tap
- Given how ubiquitous RSV is, an infant could have RSV and bacterial meningitis.
- Expert opinion: In febrile infants less than one month, do the full rule out sepsis with blood, urine, and CSF studies.
- Editor’s Note: Audio states the prevalence of meningitis is 0.4% in the first month of life. A recent systematic review of febrile infants found the risk of meningitis is 1% in the first month and 0.4% in the second month of life (Biondi et al. JAMA Netw Open. 2019)
- One study tried to determine if having RSV lowered the risk of having meningitis, but it was not powered to detect a statistically significant difference (Levine et al. Pediatrics. 2004).
- Delay in antibiotics for meningitis is associated with loss in IQ, seizure, and death (Pruitt et al. J Pediatr. 2018 and Bodilsen et al. BMC Infect Dis. 2016).
- Editor’s note: See “Things we do for No Reason: Lumbar Puncture in Low-Risk Febrile Infants with Bronchiolitis” for more.
Evaluation for other bacterial causes of fever
- Expert opinion: Obtain a UTI workup in febrile infants less than one month.
- Editor’s Note: A study of RSV-positive febrile infants <12 months found the rate of UTI was 6-7% (Kaluarachchi et al. Pediatr Emerg Care. 2014.)
- Expert opinion: No role for a blood culture in a well appearing but febrile infant >2 months (see above).
Oxygen
- Oxygen goal: AAP guidelines say 90%. Data is based on oxygen-hemoglobin dissociation curve and not on clinical outcomes.
- Editor’s Note: Continuous pulse ox is not necessary per the AAP guidelines. Despite this, almost half of admitted children (not on supplemental oxygen or nasal cannula) are placed on continuous pulse ox (Bonafide et al. JAMA. 2020).
Hospital Level of Care
- Mortality is rare in bronchiolitis in healthy kids (Doucette et al. PLoS One. 2016)
- Expert Opinion: When you need to escalate care, remember no medication will make bronchiolitis better. Open up your differential diagnosis (e.g., sepsis, pneumonia, or spontaneous pneumothorax) and consider further work-up (e.g., chest x-ray, blood gas, or blood culture).
In the infant who looks very bad, don’t miss compensated or decompensated shock. And treat it when detected.
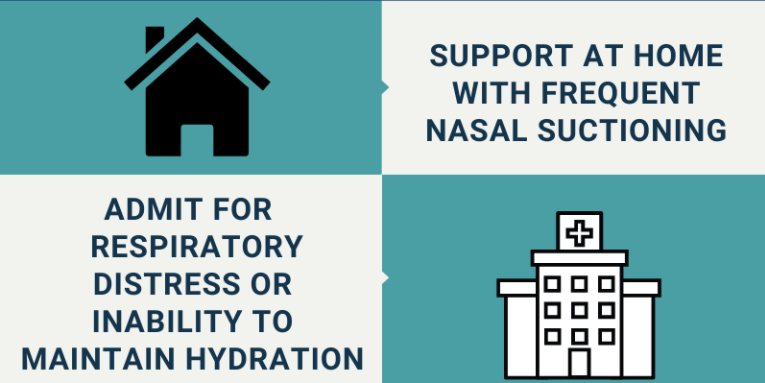
Admission criteria
- Respiratory distress: Can be hard to define, but if you’re concerned about a patient, send them into the hospital to be evaluated.
- Hydration status: Assess with a good history. If a patient is making good wet diapers, they are likely well hydrated.
Outpatient Management
Things to Do at Home
- Expert opinion: Nasal suctioning: parent-activated nasal suctioning device (ex. Nose Frida). Spray saline and then the parent sucks the mucus out (there is a filter so it does not go in the parent’s mouth). Works better than the little blue bulb. Suction every few hours, especially before feeds.
- One study showed both deep suctioning and lapses of greater than 4 hours in nasal suctioning were associated with longer LOS (Mussman et al. JAMA Pediatr. 2013).
A few last pearls…
Hydration: NG Tube vs IV fluids?
- Expert opinion: Prefer NG tube. Involve parents in the decision
- In older kids who can rip out NGT, may want to choose IV