See also
Today, I link to, excerpt from, and excerpt from The Curbsiders‘ “#398:Live! From SHM: Inpatient Cirrhosis Management”.*
*Amin M, Trubitt ME, Sata SS. “#398 SHM Live! Inpatient Cirrhosis Management”. The Curbsiders Internal Medicine Podcast. thecurbsiders.com/category/curbsiders-podcast Final publishing date June 5, 2023.
All that follows is from the above resource.
Show Segments
- Intro
- Austin Picks of the week
- Case
- Ascites
- Portal Vein Thrombosis
- AKI/HRS
- SBP
- Diuretic Management
- Albumin
- Case
- HRS treatment
- GIB Management
- Hepatic Encephalopathy Management
- Palliative Care
- Outro
Acute Liver Disease Management Pearls
- Every patient who presents to the emergency department with ascites should undergo diagnostic paracentesis.
- If a patient is not improving on empiric treatment of SBP within the first 48 hours, a repeat diagnostic paracentesis may be indicated.
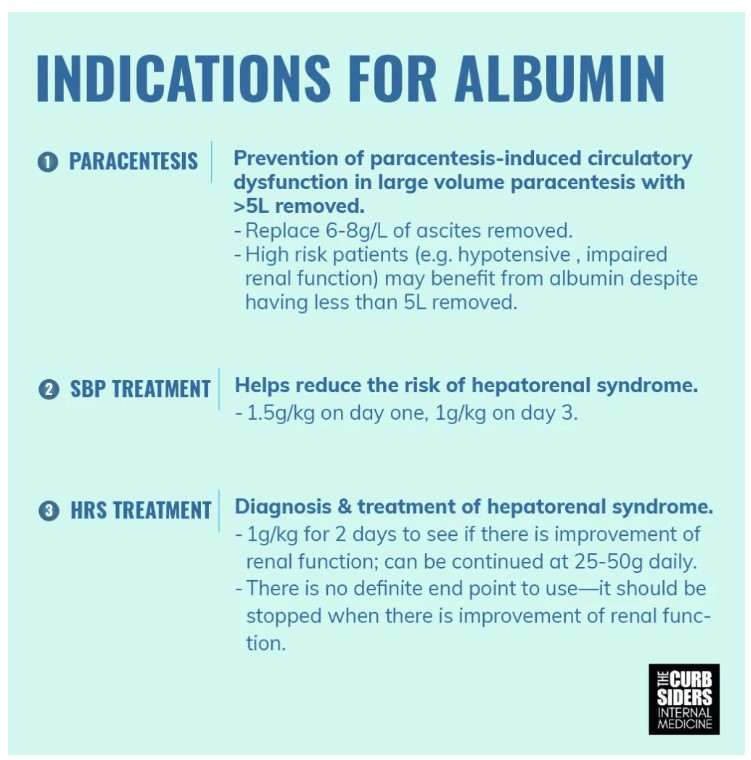
- There are 3 evidence-based indications for use of albumin in patients with cirrhosis: prevention of paracentesis induced circulatory dysfunction, treatment of SBP (in combination with antibiotics) and diagnosis/treatment of AKI/HRS.
- Treatment of acute hepatic encephalopathy should involve increasing the patient’s home lactulose regimen.
- A palliative approach to patients with cirrhosis can and should be employed at any stage of disease.
Inpatient Cirrhosis Management
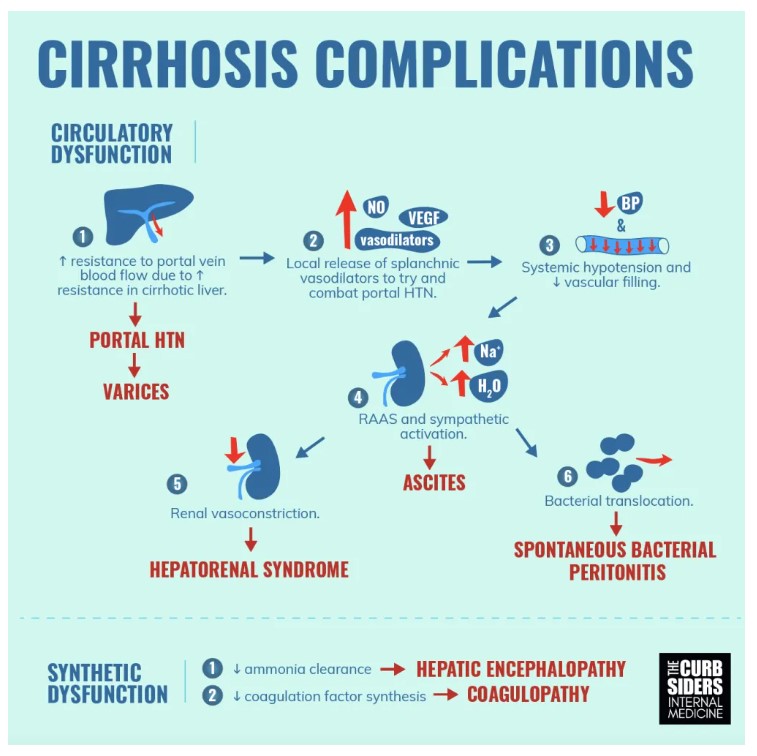
Work up and management of complications of cirrhosis
Ascites
Pathophysiology
Ascites is a result of decreased vasodilation peripherally which can lead to decreased blood flow to the kidneys. This leads to RAAS system activation which ultimately leads to salt and water retention (Biggins, 2021).
Diagnosis
Ascites is a sign of increasing hypertension of the portal venous system and is often triggered by something that has changed with the patient. As such, a systematic approach should be taken when evaluating a patient with new onset ascites. For this, Dr. Sata reminds us that taking a good history is always key. Then, work up should include liver and renal function labs, serum and urine electrolytes, and ruling out a portal vein thrombosis via CT scan or right upper quadrant ultrasound with dopplers (Biggins, 2021).
The next step in evaluation should be a diagnostic paracentesis. When doing a diagnostic paracentesis, checking a serum ascites albumin gradient is important to determine if ascites is from cirrhosis. By definition, a gradient greater than 1.1g/dL means a transudate which suggests liver etiology at 97% accuracy (Biggins, 2021). A total fluid protein >2.5g/dL suggests a cardiac etiology (Biggins, 2021).
Management
Sodium and fluid restriction are important in management of ascites. Diuretics are the mainstay of treatment of ascites. Based on physiology mentioned earlier, the RAAS system should be the main target for diuresis. Spironolactone is the initial diuretic of choice in cirrhosis, as it directly inhibits the RAAS activation. If needed, furosemide can be added to maintain potassium balance. The recommended ratio to maintain potassium balance is 100mg spironolactone to 40mg furosemide (max doses are 400mg and 160mg respectively) (Biggins, 2021).
Spontaneous Bacterial Peritonitis
Pathophysiology
Bacterial infections are more prevalent in patients with cirrhosis than the general population. This is hypothesized to be secondary to depressed immune systems and bacterial translocation from the gut to the bloodstream (Biggins, 2021).
Diagnosis and Management
Spontaneous bacterial peritonitis (SBP) must be ruled out by diagnostic paracentesis in all patients who present with ascites. This includes new onset ascites as well as any other patient with previously known ascites regardless of presence of signs and symptoms of SBP (Biggins, 2021). Dr. Sata reminds us this is because SBP is a cellular diagnosis not a clinical one (Biggins, 2021).
Bacteria in ascites is not required to make the diagnosis of SBP (can be culture negative). This is because the sample size of fluid is small compared to the overall amount of ascites. Dr. Sata says that if there is a low amount of bacteria in the fluid, there is a chance that that small amount does not contain the bacteria in it. Notably, if the paracentesis is performed before antibiotics are given, and utilize 10mL blood culture bottle for sample of ascitic fluid, there is at least 90% sensitivity for identifying the organism (Biggins, 2021).
Even in the absence of culture positive fluid, there will be a high cellular response to the presence of bacteria. Finding greater than 250 PMNs is the definition of SBP (Biggins, 2021). Once found, it should be treated with third generation cephalosporins for five to seven days. If a patient isn’t getting better after 48 hours, it is possible there is a resistant organism (commonly MDROs). In these cases, you can switch antibiotics and/or repeat a diagnostic paracentesis to try to get culture data (Biggins, 2021).
Prophylaxis
Because of the increasing prevalence of MDROs, AASLD guidelines have more stringent criteria for who should receive prophylaxis for SBP. Patients who have recovered from an episode of SBP, who have cirrhosis and a concurrent GIB, who have low protein and renal dysfunction (Cr > 1.2, BUN > 25, Na < 130) or liver failure (Child Pugh > 9 or bilirubin > 3) should receive prophylaxis with ciprofloxacin or norfloxacin (Biggins, 2021). And while some experts recommend trimethoprim-sulfamethoxazole, the formal guidelines do not make that recommendation due to sparse data (Biggins, 2021).
Portal Vein Thrombosis/Coagulopathy
Pathophysiology
Cirrhosis results in a complex coagulability picture in which patients have both procoagulant and anticoagulant tendencies. Portal vein thrombosis (PVT) specifically is defined by the presence of a thrombus in the lumen of the portal vein that can extend into the intrahepatic and extrahepatic branches (Senzolo 2021).
Diagnosis
By history, patients with PVT may present with components of Virchow’s triad—decreased portal vein flow, hypercoagulability, and damage to the vessel wall. Initial evaluation for PVT is done by ultrasound with Doppler and confirmed and staged with cross sectional imaging via CT-angio or MR-angio (Senzolo 2021).
Management
There is an inherent risk to anticoagulating a patient with cirrhosis because they are both high bleeding risk but also high risk for clotting (Senzolo 2021). Due to these risks, it is important to determine how clinically significant the clot is before starting therapeutic anticoagulation. Things to consider include whether or not the thrombus is big enough to be causing ascites that cannot be managed by diuretics. Even with these considerations, a patient centered approach with shared decision making should be implemented. Dr. Sata also recommends asking for a hepatologist’s opinion.
If you determine a patient should receive anticoagulation, heparin is appropriate in the inpatient setting. They can be transitioned to low molecular weight heparin or warfarin (Senzolo 2021). Data for DOACs is scant. (Senzolo 2021)
High value care is important. When considering INR in the setting of cirrhosis, it is important to note that it is not a true marker of clotting function (Crowe 2021). INR reflects liver synthesis dysfunction. Guidelines do not support routine administration of FFP or platelets before a diagnostic paracentesis .Dr. Sata reminds us that true clotting function would require checking a rotational thromboelastography*.
*Basic Principles of Rotational Thromboelastometry (ROTEM®) and the Role of ROTEM—Guided Fibrinogen Replacement Therapy in the Management of Coagulopathies. Diagnostics (Basel). 2023 Oct; 13(20): 3219. Published online 2023 Oct 16. doi: 10.3390/diagnostics13203219 [PubMed Abstract] [Full-Text HTML] [Full-Text PDF]
Acute kidney injury/hepatorenal syndrome
Definition
HRS is defined by cirrhosis with AKI, absence of shock, no current use of nephrotoxic medications, no signs of structural renal injury and no response after two consecutive days of diuretic withdrawal and volume expansion (Biggins, 2021).
Management
The keys to treating AKI in cirrhosis include stopping home diuretics in patients who are on them and then volume expand (see albumin section below). Next, Dr. Sata uses the mnemonic MAO (midodrine, albumin octreotide) to remember how to manage HRS-AKI. In addition to hypovolemia, there can also be systemic hypotension from portal hypertension. In these cases, octreotide (50mcg bolus, then 50mcg/hr drip) can help shunt blood back into the circulation (Biggins, 2021). Midodrine (5 to 15mg every 8 hours) is an oral vasoconstrictor that is given to support peripheral blood pressure (Biggins, 2021). Terlipressin is another vasoconstrictor used to shunt blood to the kidneys. Note that this only recently got approved in the United States (FDA Approval Announcement), and so may not be accessible nor affordable in your local hospital . Norepinephrine has also been shown to have better outcomes than midodrine/octreotide, though data is not as robust as it is for terlipressin (Biggins, 2021). Dr. Sata notes that while norepinephrine and terlipressin have higher rate of reversal of HRS, resources are limited and this has to be considered when selecting treatment.
Dr. Sata says that when thinking about using all three interventions versus a simple albumin challenge, it is important to consider the etiology of the AKI. If volume depletion seems most likely, albumin alone can be given. If the patient does not improve or worsens, or has a severe AKI with low urine sodium, midodrine/octreotide can be given.
(Biggins, 2021) & (Sata 2021).
Variceal Bleeds
Pathophysiology
Variceal bleeds are the result of increased portal hypertension. Initially, increased portal hypertension yields formation of collaterals. Concurrently splanchnic vasodilation occurs and eventually leads to further increases in portal venous inflow (Garcia-Tsao 2017).
Management
Ideally, GI should perform EGD with potential intervention no later than 12 hours after presentation (Garcia-Tsao 2017). In the meantime, hospitalists should support the patient’s blood pressure—hold diuretics and beta blockers, resuscitate with a restrictive transfusion strategy (hgb 7-9) (Garcia-Tsao 2017). When compared to a more liberal strategy (hgb 9-11 g/dL), there were lower rates of rebleeding and mortality with the restrictive strategy (Garcia-Tsao 2017). You should also give SBP prophylaxis in these situations as patients with variceal bleeds are at high risk for developing SBP. The recommended prophylaxis is IV ceftriaxone for no more than 7 days. (Garcia-Tsao 2017)
Prophylaxis
Once a patient has had and subsequently recovered from an acute variceal bleed, secondary prevention with non selective beta blockers (propranolol, nadolol) should be considered. Notably patients have a 60% risk of rebleeding the first year after an acute variceal bleed (Garcia-Tsao 2017). Dr. Sata reminds us that , the patient’s blood pressure should be able to tolerate the non-selective beta blocker if initiating.. Along those lines, carvedilol has been shown to be effective in some trials, but must be used with caution due its significant blood pressure effects (Singara 2014).
Hepatic Encephalopathy
Normally, the liver aids in clearance of toxins such as ammonia. In cirrhosis, there is a decrease in elimination of ammonia which leads to hepatic encephalopathy (HE).
Diagnosis
HE can present in a variety of way with nonspecific neurological and psychiatric manifestations (Vilstrup 2014). This is a clinical diagnosis that requires excluding other potential causes of encephalopathy (Vilstrup 2014). Ammonia levels do not need to be checked to prove a patient has hepatic encephalopathy (Vilstrup 2014).
Management
The treatment is nonabsorbable disaccharide (lactulose is most commonly used)(Vilstrup 2014). Dr. Sata likes to think of dosing for lactulose in inpatient management of acutely worsened HE similar to the way we would treat heart failure. Specifically, that if a patient comes in volume overloaded (or in this case, encephalopathic), you should not merely continue their home dose. An increase in dose is required to be effective. Increased frequency is the key. Rifaximin, L-ornithine L-aspartate and zinc are also used (Vilstrup 2014).
Palliative Approach to Cirrhosis
Quality of life is severely affected by cirrhosis. As such, palliative care should be considered and provided at any stage of illness (Rogal 2022) Dr. Sata says that it is important to discuss the prognosis, morbidity and mortality with the patient. Often, patients are not aware of the true severity of illness. As a result, they may not know that palliative measures may be appropriate for them.
Symptom management
Pain can be mechanical, inflammatory or non-liver pain. Chronic pain management in patients with cirrhosis should include both pharmacologic and non-pharmacologic modes of treatment. Acetaminophen can be given up to 2g daily. NSAIDs, however should be avoided given increase risk of renal injury, bleeding and ascites. Opioids can be used with caution as patients with liver disease at high risk for opioid related adverse events (Rogal 2022).
For muscle cramps—baclofen, taurine, vitamin E can be used (Rogal 2022)
For pruritus topical creams, antihistamines and cholestyramine (Rogal 2022) .