In this post, I link to and excerpt from The Fourth E-Exit From The “5Es” of emergency physician-performed focused cardiac ultrasound: a protocol for rapid identification of effusion, ejection, equality, exit, and entrance [PubMed Abstract] [Full-Text HTML] Full-Text PDF]. Acad Emerg Med. 2015 May;22(5):583-93.
All that follows is from the above resource.
Abstract
Emergency physician (EP)-performed focused cardiac ultrasound (EP FOCUS) has been increasingly recognized as a crucial tool to help clinicians diagnose and treat potentially life-threatening conditions. The existing literature demonstrates a variety of EP FOCUS applications and protocols; however, EP FOCUS is not taught, practiced, or interpreted consistently between institutions. Drawing on over 12 years of experience in a large-volume, high-acuity academic emergency department, we have developed a protocol for teaching and performing EP FOCUS known as “The 5Es,” where each E represents a specific assessment for immediately relevant clinical information. These include pericardial effusion, qualitative left ventricular ejection, ventricular equality, exit (aortic root diameter), and entrance (inferior vena cava diameter and respirophasic variation). Each of these assessments has been well described in the emergency medicine literature and is within the scope of EP-performed echocardiography. This approach provides a reliable and easily recalled framework for assessing, teaching, and communicating EP FOCUS findings that are essential in caring for the patient in the emergency setting.
It has been recognized for more than 25 years that emergency physician (EP)-performed focused cardiac ultrasound (EP FOCUS) is an important skill for the care of patients with potentially life-threatening presentations.1, 2 A recent review detailed 16 specific protocols that included cardiac ultrasound (US) as part of the point-of-care US assessment in medical shock.3 The term “focused cardiac ultrasound” has been addressed in some detail (FOCUS,4 FCU,5 and FoCUS6). However, this term is not specialty-specific, may include assessments that are not relevant in the acute/emergency setting, and has not included assessment of the thoracic aortic root (“exit”), which may be particularly applicable to acute and emergent presentations. We have found that the proximal thoracic aorta can be reliably assessed, providing vital information about potential aortic pathology in patients presenting with acute symptoms.7 We thus propose the “5Es” to assess for the presence of a pericardial effusion, left ventricular ejection, ventricular equality, exit (aortic root diameter), and entrance (inferior vena cava [IVC] diameter and respirophasic variation). The 5Es protocol provides an easy-to-teach, evidence-based, and standardized approach to EP FOCUS for the rapid identification and management of time-sensitive pathologic conditions. Approach to exam
Typically EP FOCUS uses one or more of three windows and five views: a parasternal long-axis (PSLA), a parasternal short-axis (PSSA), an apical four-chamber (A4C), a subcostal long-axis (SCLA), and a subcostal four-chamber (SC4C) view. While pertinent findings are optimally confirmed in at least two views, it is understood that time constraints, patient acuity, patient mobility, and patient habitus may limit views.6, 8 For images in this article, we will use an emergency medicine convention for cardiac imaging with the probe marker oriented to the patient’s right, which keeps the anatomic right on the screen-left, as is the convention for other US imaging.9 This is in contrast with image and probe orientation utilized in traditional cardiology-performed US, but has been recognized as an accepted convention that we find to be conceptually easier, particularly when performing EP FOCUS as part of an integrated examination such as the focused assessment with sonography for trauma (FAST) or the rapid US for shock and hypotension.3, 6
As has been discussed previously in the emergency US literature, EP FOCUS is not intended to replace comprehensive echocardiography (echo) when more thorough cardiology evaluation is indicated. The clinical questions addressed by EP FOCUS tend to be limited and qualitative but it should be understood that EP FOCUS findings may fall on a spectrum that can make binary categorization challenging. The EP is encouraged to use professional judgment for the interpretation and integration of his or her findings into the diagnosis and care of the patient, as well as the need for specialist consultation.
Exit
The fourth “E” in our protocol is for exit from the heart, or the assessment of the aortic root for thoracic aortic aneurysm, and thoracic aortic dissection (TAD). Aneurysmal disease of the thoracic aorta predisposes to aortic dissection.49 TAD is a time-dependent and potentially deadly disease process that can present silently or masquerade as a variety of clinical presentations. TAD results from a tear in the intima of the aorta that can propagate in either an anterograde or a retrograde fashion. Retrograde dissections can produce a number of US findings such as an intimal flap, aortic valve insufficiency, retrograde aortic flow, or rupture into the pericardium with pericardial effusion and tamponade. While contrast enhanced computed tomography (CT) remains the test of choice for diagnosing thoracic aortic disease, transthoracic echo has been shown to be accurate for detection of aortic root dilation and may be performed rapidly with a high degree of specificity by the EP at the bedside in a patient presenting with acute chest pain and/or hemodynamic instability.7, 50
Exit
The fourth “E” in our protocol is for exit from the heart, or the assessment of the aortic root for thoracic aortic aneurysm, and thoracic aortic dissection (TAD). Aneurysmal disease of the thoracic aorta predisposes to aortic dissection.49 TAD is a time-dependent and potentially deadly disease process that can present silently or masquerade as a variety of clinical presentations. TAD results from a tear in the intima of the aorta that can propagate in either an anterograde or a retrograde fashion. Retrograde dissections can produce a number of US findings such as an intimal flap, aortic valve insufficiency, retrograde aortic flow, or rupture into the pericardium with pericardial effusion and tamponade. While contrast enhanced computed tomography (CT) remains the test of choice for diagnosing thoracic aortic disease, transthoracic echo has been shown to be accurate for detection of aortic root dilation and may be performed rapidly with a high degree of specificity by the EP at the bedside in a patient presenting with acute chest pain and/or hemodynamic instability.7, 50
With respect to aortic dissection, dynamic images of the ascending aorta may detect an intimal flap seen as a hyperechoic linear structure within the aortic lumen that moves with each heartbeat. While the sensitivity of TTE for intimal flap is low, its visualization carries a high specificity.50 Furthermore, a retrograde flap may cause aortic insufficiency and/or bleeding into the pericardium. The presence of aortic root dilation and/or intimal flap with a pericardial effusion should prompt immediate consultation to cardiothoracic surgery, with CTA if the patient will tolerate it.
Pearls and Pitfalls of Exit
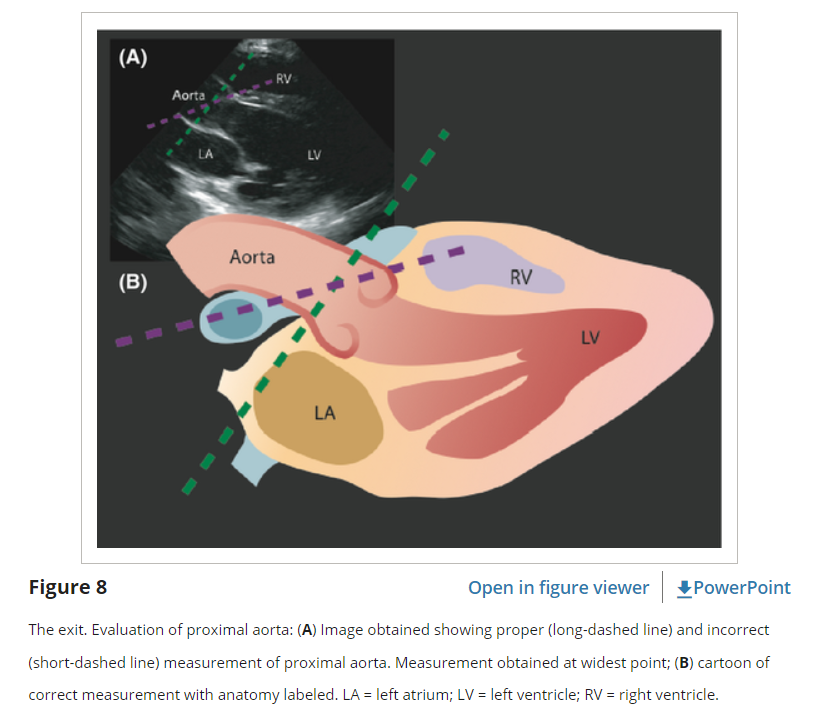
A common error occurs when practitioners place their measurement cursors parallel to the edge of the US footprint rather than perpendicular to the long axis of the vessel. This results in oblique measurements that can overestimate the true aortic diameter (Figure 8).
While the “exit” of EP FOCUS reliably assesses the proximal aortic root, thoracic aortic dilatation or an intimal flap may occur distal to the aortic root. Assessment of other parts of the thoracic aorta may be enhanced by using a suprasternal notch window and by visualizing portions of the descending aorta, often seen in the far field on the PSLA view.
Mirroring and reverberation artifacts can mimic intimal flaps.51 To avoid errors in interpretation of intimal flaps, the examiner should interrogate the aorta from multiple angles and transducer locations, look for flap motion independent of surrounding structures, ensure that the structure is confined to the lumen, and use Doppler to demonstrate differential flow on either side of the flap.
Thoracic aortic dilatation is strongly associated with dissection; however, there can be aneurysm without dissection and dissection without aneurysm.49 The presence of thoracic aortic dilatation should prompt greater suspicion of thoracic aortic disease, but its absence should not rule it out. If there is suspicion of disease, CTA remains the diagnostic test of choice, particularly if the patient is hemodynamically stable. Early EP FOCUS may prompt and expedite appropriate diagnostic testing and consultation when needed.50