In this post, I link to and excerpt from The Third E-Equality From The “5Es” of emergency physician-performed focused cardiac ultrasound: a protocol for rapid identification of effusion, ejection, equality, exit, and entrance [PubMed Abstract] [Full-Text HTML] Full-Text PDF]. Acad Emerg Med. 2015 May;22(5):583-93.
All that follows is from the above resource.
Abstract
Emergency physician (EP)-performed focused cardiac ultrasound (EP FOCUS) has been increasingly recognized as a crucial tool to help clinicians diagnose and treat potentially life-threatening conditions. The existing literature demonstrates a variety of EP FOCUS applications and protocols; however, EP FOCUS is not taught, practiced, or interpreted consistently between institutions. Drawing on over 12 years of experience in a large-volume, high-acuity academic emergency department, we have developed a protocol for teaching and performing EP FOCUS known as “The 5Es,” where each E represents a specific assessment for immediately relevant clinical information. These include pericardial effusion, qualitative left ventricular ejection, ventricular equality, exit (aortic root diameter), and entrance (inferior vena cava diameter and respirophasic variation). Each of these assessments has been well described in the emergency medicine literature and is within the scope of EP-performed echocardiography. This approach provides a reliable and easily recalled framework for assessing, teaching, and communicating EP FOCUS findings that are essential in caring for the patient in the emergency setting.
It has been recognized for more than 25 years that emergency physician (EP)-performed focused cardiac ultrasound (EP FOCUS) is an important skill for the care of patients with potentially life-threatening presentations.1, 2 A recent review detailed 16 specific protocols that included cardiac ultrasound (US) as part of the point-of-care US assessment in medical shock.3 The term “focused cardiac ultrasound” has been addressed in some detail (FOCUS,4 FCU,5 and FoCUS6). However, this term is not specialty-specific, may include assessments that are not relevant in the acute/emergency setting, and has not included assessment of the thoracic aortic root (“exit”), which may be particularly applicable to acute and emergent presentations. We have found that the proximal thoracic aorta can be reliably assessed, providing vital information about potential aortic pathology in patients presenting with acute symptoms.7 We thus propose the “5Es” to assess for the presence of a pericardial effusion, left ventricular ejection, ventricular equality, exit (aortic root diameter), and entrance (inferior vena cava [IVC] diameter and respirophasic variation). The 5Es protocol provides an easy-to-teach, evidence-based, and standardized approach to EP FOCUS for the rapid identification and management of time-sensitive pathologic conditions.
Approach to exam
For images in this article, we will use an emergency medicine convention for cardiac imaging with the probe marker oriented to the patient’s right, which keeps the anatomic right on the screen-left, as is the convention for other US imaging.9 This is in contrast with image and probe orientation utilized in traditional cardiology-performed US, but has been recognized as an accepted convention that we find to be conceptually easier, particularly when performing EP FOCUS as part of an integrated examination such as the focused assessment with sonography for trauma (FAST) or the rapid US for shock and hypotension.3, 6
As has been discussed previously in the emergency US literature, EP FOCUS is not intended to replace comprehensive echocardiography (echo) when more thorough cardiology evaluation is indicated. The clinical questions addressed by EP FOCUS tend to be limited and qualitative but it should be understood that EP FOCUS findings may fall on a spectrum that can make binary categorization challenging. The EP is encouraged to use professional judgment for the interpretation and integration of his or her findings into the diagnosis and care of the patient, as well as the need for specialist consultation.
Equality
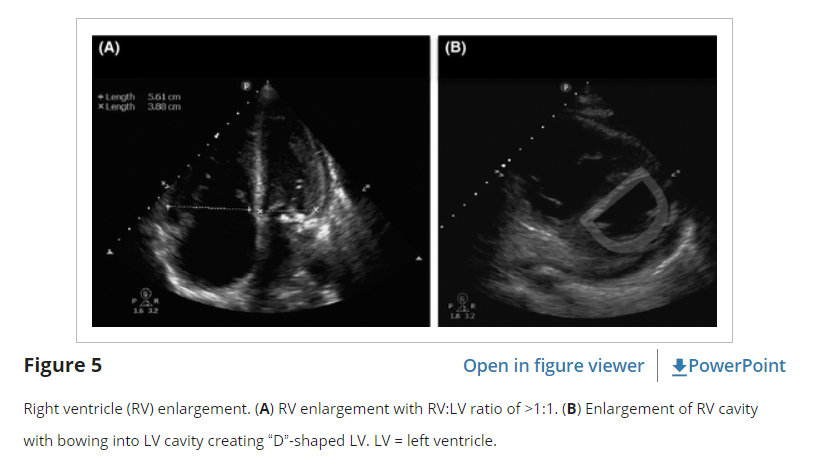
The third “E” in our protocol is for equality, referring to the relative size of the RV to the LV. In healthy patients, the RV is a low-pressure, thin-walled, high-compliance chamber that is wrapped anteriorly around the muscular, cone-shaped LV. The normal RV systolic pressure is approximately 25 mm Hg with an RV:LV diameter ratio of less than 0.6:1. When pressure in the pulmonary artery rises, the RV will dilate (Figure 5). While not perfectly sensitive, using “equality” (i.e., a 1:1 ratio) as the cutoff ensures specificity for detecting true RV strain by EP FOCUS.33, 34
Right ventricle dilatation may be acute, chronic, or acute-on chronic. However, in patients presenting with undifferentiated chest pain, shortness of breath, hypotension, or syncope, the presence of any RV dilatation should raise the diagnostic suspicion of an acute pulmonary embolism (PE). PEs can range in severity from small subsegmental disease with minimal morbidity and mortality, to massive with resultant RV failure, shock, and death. PEs are typically defined as “massive” when sustained hypotension ensues. The remaining PE categories are stratified into “submassive,” when there are signs of RV strain on echo, versus “low-risk” (also labeled “small” or “minor”), when there is no RV strain.35 EP FOCUS can help stratify these patients, with RV hypokinesis being an independent predictor of mortality.36 The presence of RV strain in suspected massive PE or diagnosed submassive PE may signal the need for more aggressive therapy such as thrombolysis or thrombectomy.35, 37–39
Techniques for Assessing Equality
When the A4C view is properly obtained, with all four chambers visible and divided by a vertically oriented interventricular septum, ventricular size can be accurately compared either qualitatively or quantitatively (Figure 5). If measured, ventricular size should be obtained between endocardial borders at the tips of the valves in diastole. However, the A4C may be technically challenging to obtain correctly. The PSLA window may show a prominent and hypokinetic anterior chamber when RV strain is present. However, tilting of the plane in the PSLA (known as the “tricuspid tilt”) may cut across the RV obliquely causing overemphasis of the RV relative to the LV and should be used with caution. On the other hand, the PSSA at the level of the papillary muscles can often provide an excellent and reliable estimation of RV:LV ratio. In the PSSA view, the greatest chamber diameters for both the RV and the LV are usually visible side by side at the level of the papillary muscles. When RV pressure rises the septum will be pushed toward the LV. The PSSA is thus the preferred view to demonstrate this septal flattening, resulting in the characteristic “D-shaped” LV (Figure 5).40 The subxiphoid view may also show RV enlargement, but should be used with caution as the RV may be overemphasized if the plane of the US cuts through it obliquely, and RV size should be confirmed in other planes.
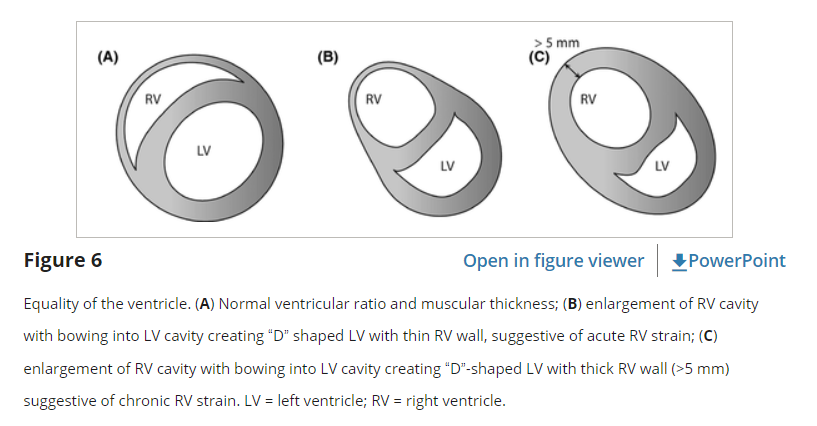
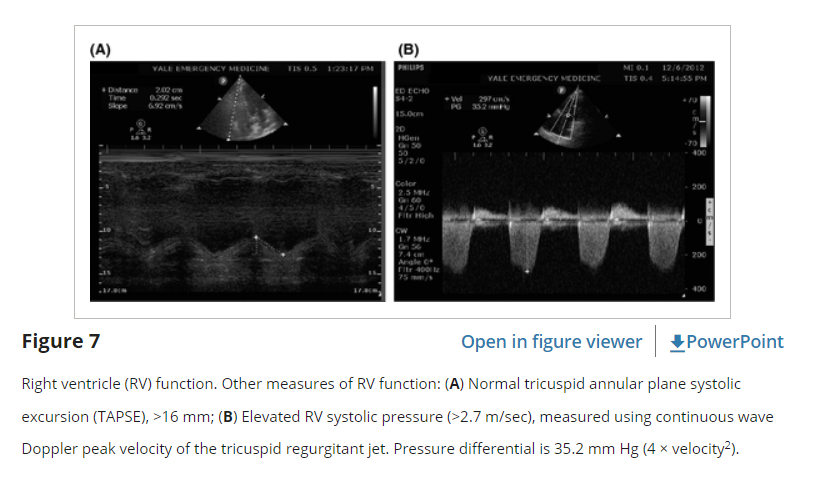
In addition to enlargement, EP FOCUS may show RV hypokinesis or be used to measure elevated RV pressure. While the LV tends to contract circumferentially and perpendicular to the long axis of the heart, the RV tends to move longitudinally, from base to apex. The A4C is the best view to demonstrate the movement of the tricuspid annulus during RV systole, allowing assessment and measurement of tricuspid annular plane systolic excursion (TAPSE, Figure 6). A TAPSE of 18 mm or greater is typically considered normal.41 TAPSE is a technique for assessing RV function that is well described in the cardiology literature, but to our knowledge only described once in the EP literature.42–45 In our experience it is easily measured when an adequate A4C view is present and has been described as reproducible and perhaps better than RV size as a predictor of PE severity.41, 43, 45
Right ventricle systolic pressure may be estimated quantitatively when tricuspid regurgitation is present. The peak velocity of the tricuspid regurgitant jet should be measured using continuous wave spectral Doppler with the Doppler signal in line with the jet (typically in an A4C view). The pressure difference between the RV and RA can then be estimated using the modified Bernoulli equation, with ΔP = 4 × V2. A velocity greater than 2.7 m/sec typically indicates elevated RV systolic pressure (Figure 6), with velocities of 4 m/sec or greater indicating chronic RV pressure overload.
Pearls and Pitfalls of Equality
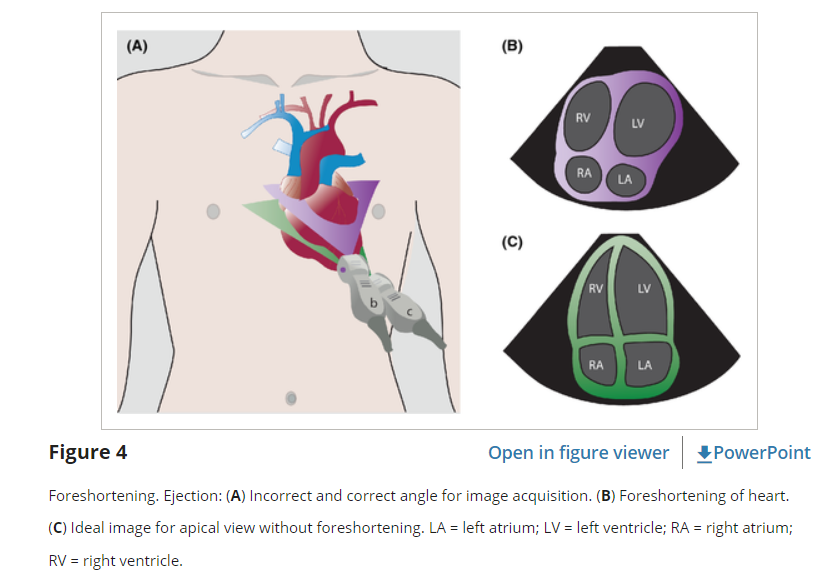
One of the primary pitfalls of RV assessment is overestimation of RV to LV ratio (false-positive) based on the US plane cutting through the RV in an oblique plane that makes the RV look relatively larger than the LV. This can be an issue in the PSLA, SX4C, or A4C views. For apical views, be sure to slide the probe sufficiently lateral on the chest wall so that the probe lies over the point of maximum intensity and true apex. Flattening the plane to transect through the base of the heart avoids foreshortened chambers and misinterpretation of their sizes (Figure 4). For the PSLA view it is important to fan through the long axis of the heart to make sure the LV is maximized relative to the RV.
An understanding of probe marker orientation conventions and relative probe placement on the patient is essential because if reversed, the normally larger LV may be mistaken for an abnormally enlarged RV (or an enlarged RV may be mistaken for a normal LV), especially in the A4C view.9
When imaged correctly by an EP with appropriate experience in echo, the presence of an RV:LV ratio of 1:1 or greater is highly specific for RV strain, as determined by consultant-performed echo.33, 34 However, because using a 1:1 ratio for a dilated RV sets a higher threshold (specificity) for pathology, sensitivity is sacrificed.35 Additionally, it is important to keep in mind that PEs (albeit “small”) may occur without any signs of right heart strain at all.
Right ventricle dilation may be a result of acute, chronic, or acute-on-chronic RV pressure elevation. While differentiation between these entities can be challenging, there are a few clues that may be available using both two-dimensional imaging and Doppler. With acute right heart dilation the RV wall remains thin, but over time the RV will hypertrophy. If the RV free wall myocardium measures over 5 mm, this is indicative of chronic strain (Figure 7). [TW: I believe this paragraph should refer to figure 6].
Furthermore, while both acute and chronic conditions produce measurable right heart pressure elevations, the acutely strained, thin-walled RV will not be able to generate extremely high pressures. A pressure gradient of more than 60 mm Hg (tricuspid regurgitation jet of about 4 m/sec or more) indicates chronic RV pressure elevation. McConnell’s sign, the presence of RV dilation and hypokinesis of the mid and basal portions of the RV with “apical sparing” (as opposed to global RV dysfunction), has been reported to be specific for acute RV strain, although it may not differentiate well between acute strain from PE versus acute strain from RV infarction.37, 46–48