Today I I link to and excerpt from Dr. Josh Farkas’ Internet Book of Critical Care chapter, Alcoholic Hepatitis. February 13, 2021.
And here are the direct links to the various sections of the chapter:
CONTENTS
And all that follows is from the IBCC chapter:
clinical features
clinical findings
- Common symptoms:
- Jaundice.
- Fever.
- Tender hepatomegaly.
- Nausea, vomiting, and anorexia.
- Patients may have superimposed features from underlying alcoholic cirrhosis (e.g., ascites).
- Severe disease may cause encephalopathy.
epidemiology
- Alcoholic hepatitis occurs following chronic alcoholism (e.g., >>5 years), but it can occur after shorter periods of intense exposure (e.g., >6 months).(32277902) Patients may stop drinking days or weeks prior to admission, because they feel too ill to drink.
evaluation
labs
- Transaminases are mildly-moderately elevated:
- Bilirubin is elevated, at least >3 mg/dL, and is often extremely elevated (with a median value of 13 mg/dL)(31219169)
- INR elevation is usually seen.
- Acetaminophen level should be obtained if there is any concern for ingestion.
- An extensive hepatitis panel (e.g., HAV, HBV, HCV) isn’t mandatory if there is a clear history of alcohol ingestion. If the alcohol history is unclear, then evaluation may be indicated for infectious hepatitis, autoimmune hepatitis (with antinuclear antibody and anti-smooth muscle antibody tests), or drug/toxin-induced liver injury.
- However, when initiating a prolonged course of steroid therapy, it may be wise to exclude chronic HBV or HCV infections.
right upper quadrant ultrasound with Doppler sonography
- This is mostly useful to exclude alternative diagnoses (e.g., biliary obstruction or hepatic vein thrombosis). It will also evaluate for the presence and extent of ascites.
- Alcoholic liver disease may cause hepatomegaly with fatty infiltration of the liver. However, these are nonspecific findings which, for example, may also be seen among patients with nonalcoholic fatty liver disease.
neurological investigation
- Lumbar puncture may be indicated if fever and substantial alteration of mental status are present.
- CT scan of the head may be indicated for altered mental status.
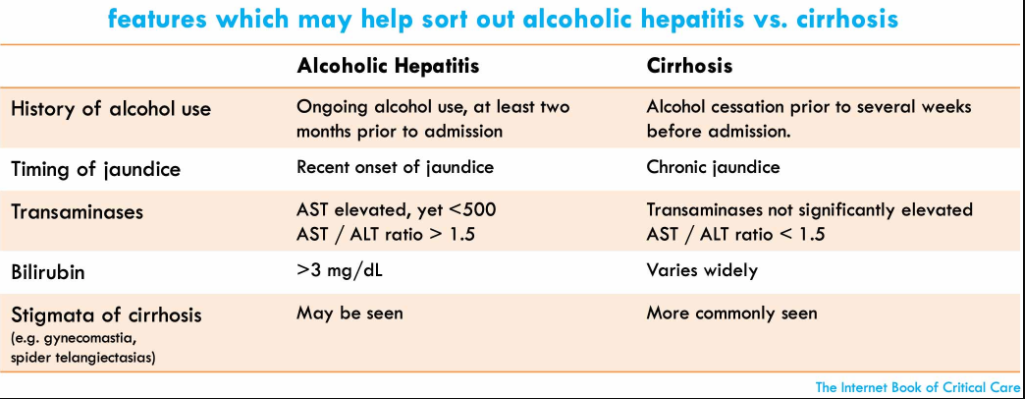
alcoholic hepatitis vs. cirrhosis
scope of the problem
- Epidemiology, signs, symptoms, and lab abnormalities are extremely similar between alcoholic cirrhosis and alcoholic hepatitis.
- Alcoholic hepatitis and alcoholic cirrhosis overlap to a large extent (e.g., the presence of cirrhosis doesn’t exclude alcoholic hepatitis).
therapeutic implications
- The management of both conditions is overall extremely similar (below), consisting primarily of supportive care.
- The only major difference between the acute management of alcoholic hepatitis versus cirrhosis is the use of steroid. The benefit of steroid in alcoholic hepatitis is controversial, so when in doubt omission of steroid may often be reasonable.
features to help sort out alcoholic hepatitis vs. cirrhosis (26921783)
management*
*Carefully review this section in the IBCC Chapter
Pitfalls
- Failure to manage other comorbid conditions occurring along with alcoholic hepatitis (e.g., Wernicke’s encephalopathy, refeeding syndrome, malnutrition).
- Incorrectly attributing multifactorial delirium to alcohol withdrawal.
- Failing to evaluate thoroughly for underlying infection (e.g., spontaneous bacterial peritonitis).