In this post I review and excerpt the teaching points from Emergency Medicine Cases‘ ECG Cases 20 – Approach to Bradycardia and the BRADI Mnemonic. Written by Jesse McLaren; Peer Reviewed and edited by Anton Helman, April 2021.
All that follows is from the above post.
In this ECG Cases blog we look at 10 patients’ ECGs* who presented with bradycardia, an approach to identify reversible causes with the BRADI mnemonic and use ECG interpretation to guide management.
Bradycardia and the BRADI mnemonic
Bradycardia/blocks range from normal variants to life threatening emergencies. As the EM Cases main episode podcast explains, the approach includes assessing stability, symptoms, ECG localization, and reversible causes.
According to a retrospective study of nearly 300 patients who presented to the ED with symptomatic bradycardia (with median ventricular rate of 33), the most common chief complaints were: syncope, dizziness, collapse, angina, and dyspnea/heart failure. The basic maneuver of laying the patient flat eliminated symptoms in 40% of bradycardic patients, while the remaining 60% received ACLS intervention(s): atropine in 80%, epinephrine or dopamine in 50%, and transcutaneous pacing in 30%. Regardless of initial management, half of all patients ultimately required a permanent pacemaker, but the other half had a reversible cause. As the article emphasized: “identification of treatable, reversible causes of the bradycardia is the key for successful management.”[1]
The ECG can localize the mechanism of bradycardia/blocks, based on the anatomy of conduction. Normal conduction begins in the SA node and depolarizes the atria (P wave), pauses in the AV node (PR interval) and then travels rapidly through the His bundle and bundle branches to depolarize the ventricles (QRS). Abnormalities can happen at any of these three levels, as outlined by the ACC/AHA guidelines [2]:
- Sinus node dysfunction
- sinus bradycardia (upright P in I/II): can be normal, vagal response, or pathological
- escape rhythm: atrial (narrow complex with different P), junctional (narrow complex with absent or retrograde P), ventricular (wide complex)
- atrial fibrillation/flutter
- AV block
- nodal: can be normal, usually self-limiting or responds to atropine
- First-degree: constant PR>200 without dropped beats
- Second-degree type 1 (Wenkebach): PR lengthening before dropped beat
- infranodal: requires pacemaker (unless from reversible cause)
- Second-dgree type 2: constant PR before dropped beat
- Third-degree: variable PR with complete heart block
- Ventricular conduction disease
- wide complex supraventricular
- hyperkalemia
- fascicular block: RBBB, LAFB, LPFB
- wide complex ventricular: idioventricular tachycardia
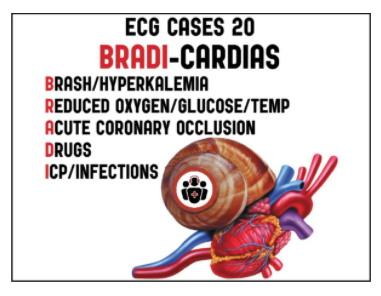
The physiology of conduction depends on coronary perfusion and metabolic conditions, and is influenced by the autonomic nervous system and medications. This outlines the list of acute reversible causes of bradycardias/blocks, which can be remembered by the mnemonic BRADI:
BRADI mnemonic for reversible causes of bradycardia
BRASH/hyperkalemia
- Isolated hyperkalemia
- BRASH syndrome (Bradycardia, Renal failure, AV node blockade, Shock and Hyperkalemia)
Reduced vital signs
- Hypoxia
- Hypoglycemia
- Hypothermia +/- hypothyroid
Acute coronary occlusion
- Inferior MI: nodal ischemia and vagal response, self-limiting or responds to atropine
- Anterior MI: infranodal ischemia, often requires pacing
Drugs: withdraw if stable, reverse if unstable
- Beta-blockers
- Calcium channel blockers
- Digoxin
Intracranial pressure, Infection (Lyme, endocarditis): treat underlying cause
This emphasizes complete vital signs, identifying ECG evidence of hyperkalemia and ischemia, withdrawing or reversing medication toxicity/overdose, and considering other dangerous causes.
Hyperkalemia is the great imitator which can cause a wide variety of ECG manifestations, including bradycardias/blocks. A study of patients with symptomatic bradycardia found that predictors of hyperkalemia included diabetes, treatment with diltiazem, bradycardia, junctional rhythm or atrial fibrillation, and peaked T waves[3]. Another study of patients with hyperkalemia found that predictors of adverse events were bradycardia, junctional rhythm, and wide QRS[4]. This study found that all patients with adverse events had preceding signs on ECG, most patients had adverse events prior to lab confirmation of potassium, but none had adverse events after treatment with calcium. So the ECG can identify hyperkalemic patients at high-risk for adverse events, which can be prevented with empiric calcium. The BRASH syndrome (Bradycardia, Renal failure, AV blockade, Shock, and Hyperkalemia) identifies a synergy of causes that can produce unstable bradycardia, and which requires comprehensive treatment.[5]