In this post, I link to and excerpt the section, management of combined anticholinergic plus sodium channel blocker toxicity, from the Internet Book of Critical Care Chapter [Link is to the Table of Content], Anticholinergic Intoxication, by Dr. Josh Farkas.
I excerpt from my study resources because doing this helps me reinforce my learning
Note to myself and to readers: Review the following before or after reviewing the material in this post:
- Dr. Josh Farkas’ outstanding IBCC chapter, Sodium Channel Blocker Toxicity (including tricyclic antidepressants), April 26, 2021
- This is an awesome resource and can’t be reviewed too often.
- Dr. Scott Weingart’s outstanding EMCrit Podcast 98 – Cyclic (Tricyclic) Antidepressant Overdose. May 14, 2013
- The podcast and show notes are a great practical review of what is discussed in Dr. Farkas’ chapter
- And finally, my post, Toxidrome Summary Graphics From Drs. Faidal And Farkas. Posted on April 18, 2021 by Tom Wade MD
Here are excerpts from management of combined anticholinergic plus sodium channel blocker toxicity and from Sodium Channel Blocker Toxicity (including tricyclic antidepressants), both from Dr. Farkas.
All that follows is from one of the two links above.
First, from Sodium Channel Blocker Toxicity (including tricyclic antidepressants)
overview – sodium channel blockers & tricyclic antidepressants
Tricyclic antidepressants (TCAs) are the perhaps the most widely discussed intoxicant which inhibits sodium channels (causing a characteristic pattern of QRS widening with a tall R-wave in aVR). However, a broad variety of other xenobiotics also block sodium channels, causing a similar pattern of findings.
TCAs are the original gangster of sodium channel blockade.
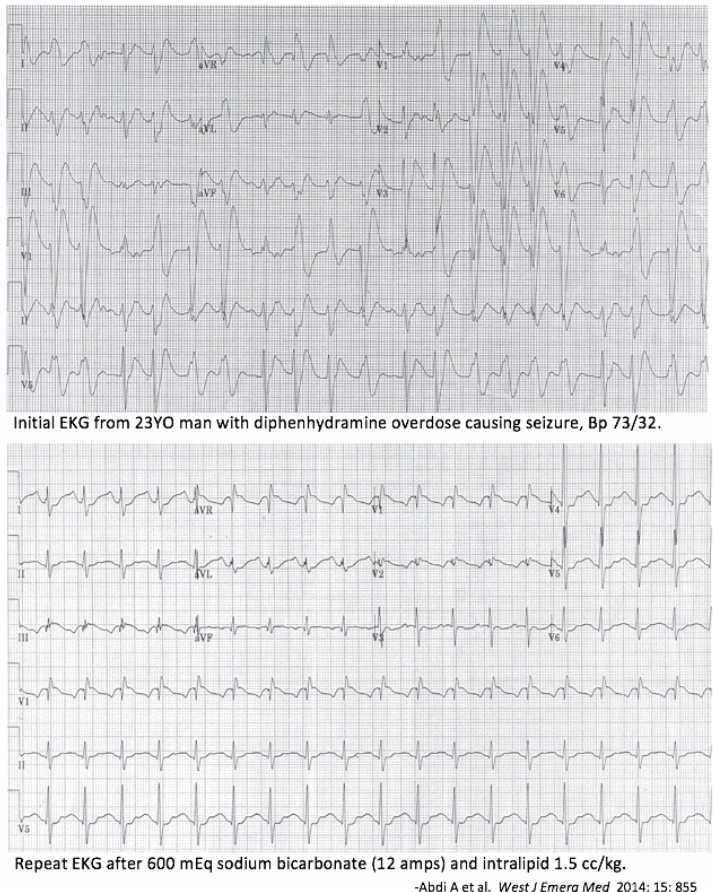
With the increased use of selective serotonin reuptake inhibitors (SSRIs), the use of tricyclic antidepressants has decreased. Consequently, TCA intoxication has become less common. Consequently, most patients who present with features of sodium channel blockade currently do not actually have TCA intoxication (but rather may have intoxication with other sodium blockers, such as cocaine or diphenhydramine).
This chapter will explore a broad approach to sodium channel blocker toxicity. Much of the data and experience have been obtained from studies of TCA intoxication, but this appears to be generalizable to other forms of sodium channel blockade.
One complicating factor here is that TCAs have numerous effects in addition to sodium channel blockade (e.g., anticholinergic effects and antihistamine effects). Consequently, some aspects of TCA intoxication are not generalizable with other sodium channel inhibitors.
EKG findings in sodium channel blockade
EKG is test of choice
- EKG is the most direct reflection of cardiac sodium channel blockade.
- EKG is the only test capable of suggesting sodium channel blockade in a patient with an unreliable or unobtainable history.
- If EKG abnormalities are suspected to be due to sodium channel blocker toxicity, two ampules (100 mEq total) of hypertonic bicarbonate should be given with a repeat EKG subsequently. Improvement in EKG findings following administration of bicarbonate supports the presence of sodium channel blockade.
- In a patient who overdosed on a medication known to block sodium channels (e.g., TCA), the EKG should be repeated frequently to allow for early detection of sodium channel toxicity.
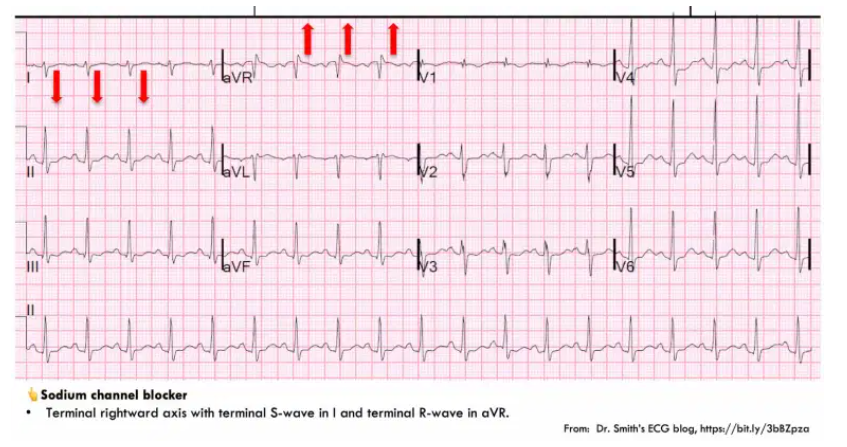
- The key to diagnosing sodium channel blockade is recognition of terminal rightward axis deviation. Electrophysiologically, this is caused by slow conduction through the myocardium, leading to delayed depolarization of the right ventricle (such that the last bit of the QRS complex points in a rightward direction). This creates the following pattern:
- (1) Deep, terminal S-wave in Lead I (which may be broad or slurred).
- (2) Terminal tall R-wave in aVR.
- The differential diagnosis of this pattern focuses on three entities: sodium channel blockade, hyperkalemia, or Brugada syndrome.
- Hyperkalemia can generally be excluded rapidly based on other features of the EKG, or laboratory studies.
- Brugada syndrome is discussed further below (but as a rule of thumb, a true Brugada Syndrome patient is extremely rare – so Brugada syndrome is a bit of a diagnosis of exclusion).
- Among patients with TCA intoxication, a tall R-wave in aVR (R-wave >3 mm or an R/S ratio >0.7) predicts seizure or arrhythmia.(7618783)
Brugada type I pattern
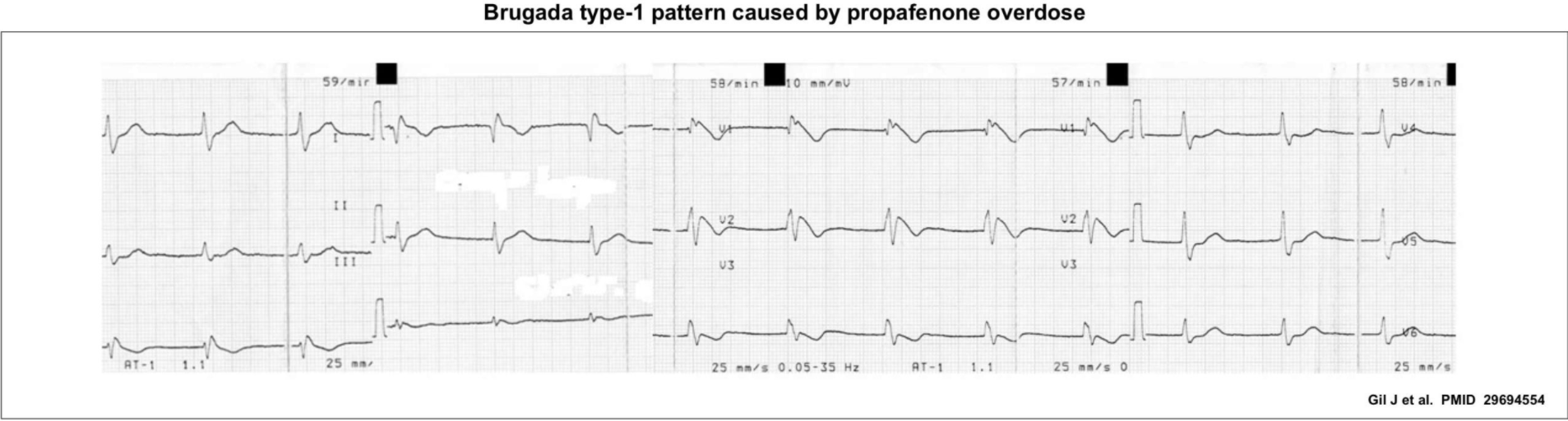
- Brugada type I pattern is marked by the following findings in V1, V2, or multiple leads within V1-V3:
- Coved ST elevation followed by T-wave inversion.
- No well-defined r’ wave.
- Gentle downslope from the QRS complex into the T-wave (this is more gradual than with right bundle branch block).
- Brugada type I pattern reflects sodium channel insufficiency, due to acquired causes and/or a genetic channelopathy. This can occur in roughly three different contexts:
- (#1) Some patients with genetic abnormalities and Brugada syndrome may have this abnormality on their baseline EKG.
- (#2) Some patients with subtle alternations of their sodium channels may manifest this EKG pattern only due to a variety of physiologic stressors (e.g., fever, hypothermia, hyperkalemia, pulmonary embolism).
- (#3) Patients with normal sodium channels may manifest this abnormality due to overdose of sodium channel blocking medications. For example, this pattern is seen in ~15% of patients with tricyclic intoxication.
- Overall, Brugada type I pattern is not diagnostic of sodium channel blocker overdose. However, the pattern should be recognized since it can support this diagnosis within the appropriate context.
*Here is the link to the Brugada Syndrome Search Results from Dr. Smith’s ECG Blog.
QRS widening
- QRS widening is not specific for sodium channel blockers, since it may be caused by a broad range of conduction abnormalities. However, QRS widening is useful because it can provide a quantitative indication of the severity of the sodium channel intoxication (assuming that the patient has a normal baseline QRS interval; whenever possible, compare the QRS to the patient’s baseline EKG).
- In the context of TCA intoxication, QRS duration has prognostic and therapeutic significance:
- In severe intoxication, the QRS complex may become profoundly broad, producing a sine wave pattern.
- Sinus tachycardia with a wide QRS interval may mimic ventricular tachycardia.
other findings which may be seen on EKG
- Sinus tachycardia is commonly seen in TCA intoxication (due to anticholinergic effects).
- Sinus bradycardia may occur with some antiarrhythmics or beta-blockers.
- QT interval may be widened, secondary to slow ventricular depolarization. However, torsade de pointes doesn’t commonly occur (perhaps because patients are commonly tachycardic).
clinical manifestations
clinical manifestations of cardiac toxicity
- Hypotension.
- Sinus tachycardia.
- Monomorphic ventricular tachycardia.
CNS effects
- Sodium channel blockers can often also penetrate the brain, with a variety of effects:
- TCAs can inhibit central GABA receptors.
- CNS sodium channels may also be affected.
- Common manifestations are delirium, agitation, sedation, coma, and especially seizures.
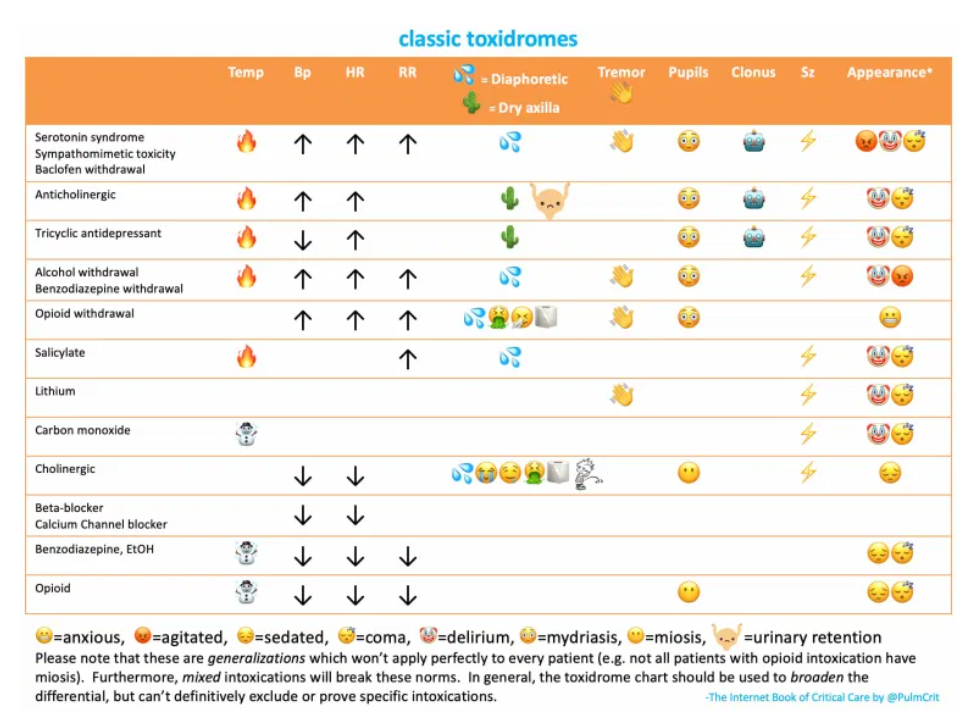
simultaneous anticholinergic toxidrome
- Many agents that block sodium channels also have anticholinergic effects (e.g., antihistamines, TCAs). These may simultaneously cause an anticholinergic toxidrome, with the following features:
- Dry, flushed skin, sometimes with hyperthermia.
- Pupillary dilation.
- Delirium, coma.
- Urinary retention.
- More on the anticholinergic toxidrome here.
What follows next is from the management of combined anticholinergic plus sodium channel blocker toxicity, from the Internet Book of Critical Care Chapter [Link is to the Table of Content], Anticholinergic Intoxication, by Dr. Josh Farkas.
basics
- Several agents inhibit both muscarinic acetylcholine receptors and cardiac sodium channels, most notably:
- First-generation antihistamines (e.g., diphenhydramine). In these patients, the overall clinical picture tends to be dominated by the anticholinergic toxidrome.
- Tricyclic antidepressants. In this case, the more life-threatening aspects of the intoxication tend to be dominated by effects on sodium channels.
- These intoxications can be diagnosed based on a combination of an anticholinergic toxidrome plus EKG findings of sodium channel blockade (more on that here). Of course, in some cases the diagnosis may also be based upon a known history of ingesting a specific agent.
- Some patients may be more susceptible to the sodium-blocking effect of antihistamines than other patients, possibly due to underlying genetic variability in their sodium channels (e.g., patients with Brugada syndrome variants). The EKG is the most accurate test to determine the physiologic impact that the intoxicant is having on an individual patient’s heart.
management
- This is overall a hybrid of the management of anticholinergic (as above) and sodium channel blocker intoxications (described here).
- Some supportive elements discussed above may be helpful in these patients (e.g., Foley catheter to relieve urinary obstruction).
- Sodium channel blockade is more worrisome than anticholinergic effects, since sodium channel blocker toxicity carries a greater mortality. Consequently, when in doubt, treatment should arguably focus more on adequate management of sodium channel inhibition (e.g., with hypertonic bicarbonate).
- Physostigmine is relatively contraindicated in this situation (although multiple authors do recommend the use of physostigmine for patients with known antihistamine intoxication who have EKG evidence of sodium channel blockade).