This post contains excerpts from Resource (1) below, 2012 revised International Chapel Hill Consensus Conference Nomenclature of Vasculitides:
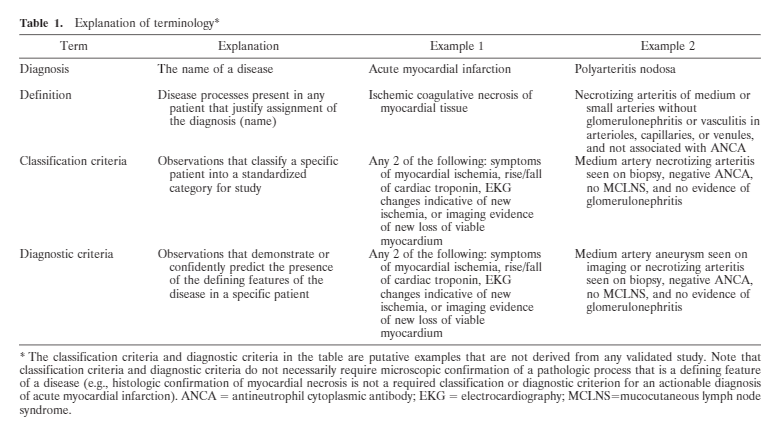
CHCC is a nomenclature system(nosology). It is neither a classification systemthat specifies what findings must be observed in a specific patient to classify that patient for clinical research nor a diagnostic system that directs clinical management (Table 1).
A disease nomenclature system specifies the name that should be used fora specifically defined disease process. A nomenclature system is constructed based on the state of knowledge at the time it is developed, and specifies the name that should be used when a patient fulfills a definition. A nomenclature system differs fundamentally from categorization systems that use identifiable classification criteria or diagnostic criteria to decide what disease definition is fulfilled by an actual patient. The name anddefinition of a disease are a given (i.e., specified in anaccepted nomenclature system), whereas diagnostic criteria and classification criteria are features that can be observed in a patient so that the presence of the disease can be inferred from this evidence. CHCC2012 nomenclature and definitions do not provide diagnostic and classification criteria, but provide a framework for inferring and rigorously verifying such criteria.
The distinction between definitions and diagnostic or classification criteria must be clear in order to understand that histopathologic terms used in definitions do not mean that a diagnosis of the disease can be made only if the pathologic process is directly observed histologically in a tissue specimen (Table 1) [above]. For example, clinically apparent mononeuritis multiplex can be a diagnostic or classification criterion for vasculitis affecting peripheral nerves without the need for a nerve biopsy in which the vasculitis is observed histologically. Likewise, in the appropriate clinical context, cavitary lung lesions documented by imaging studies can be a sufficient surrogate criterion to conclude that a patient has necrotizing granulomatous pulmonary inflammation even if tissue has not been examined histologically.
Major vasculitis categories
Vasculitis is inflammation of blood vessel walls. Inflammation of blood vessel walls at least at some time during the course of the disease is a shared defining feature of all categories of vasculitis. Some categories of vasculitis also have characteristic tissue injury unrelated to the vasculitis. Features that vary among different forms of vasculitis and can be used for categorization include etiology, pathogenesis, type of vessel affected, type of inflammation, favored organ distribution, clinical manifestations, genetic predispositions, and distinctive demographic characteristics (e.g., with respect to age,sex, race, ethnicity, and geographic distribution). Disease categorization based on etiology is often a preferred approach; however, this is not feasible for most vasculitides because the etiology is unknown. Thus, the CHCC nomenclature subdivides vasculitides based oncombinations of features that separate different forms of vasculitis into definable categories.
Vasculitides can be broadly dichotomized into infectious vasculitis, known to be caused by direct invasion and proliferation of pathogens in vessel walls with resultant inflammation, versus noninfectious vasculitis,not known to be caused by direct vessel wall invasion by pathogens. Examples of infectious vasculitis include rickettsial vasculitis, syphilitic aortitis, and Aspergillus arteritis. CHCC addresses only vasculitis that is not known to be caused by invasion of vessel walls by pathogens; however, infection is indirectly involved in the pathogenesis of some of the vasculitides addressed.One of many examples is cryoglobulinemic vasculitis caused by an autoimmune response initiated by hepatitisC virus infection.
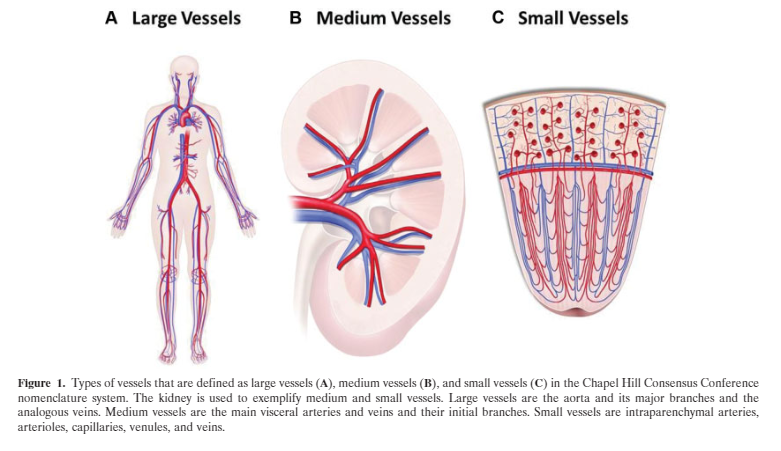
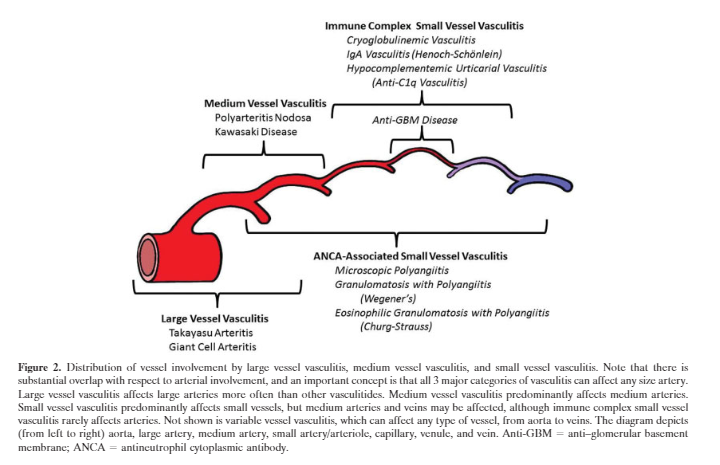
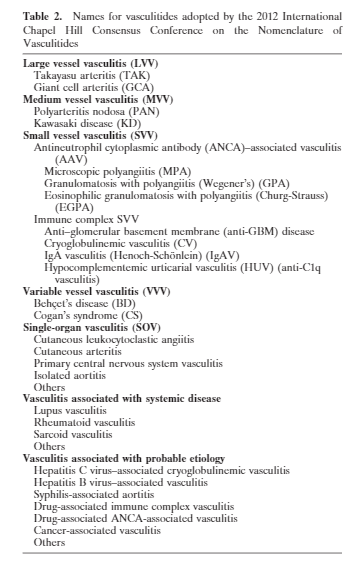
CHCC categorizes noninfectious vasculitis by integrating knowledge about etiology, pathogenesis, pathology, demographics, and clinical manifestations. The first categorization level is based on the predominant type of vessels involved, i.e., large vessel vasculitis,medium vessel vasculitis, and small vessel vasculitis(Figures 1 and 2, and Tables 2 and 3).
Table 3. Definitions for vasculitides adopted by the 2012 International Chapel Hill Consensus Conference on the Nomenclature of Vasculitides (CHCC2012)
CHCC2012 name CHCC2012 definition Large vessel vasculitis (LVV) Vasculitis affecting large arteries more often than other vasculitides. Large arteries are the aorta and its major branches. Any size artery may be affected. Takayasu arteritis (TAK) Arteritis, often granulomatous, predominantly affecting the aorta and/or its major branches. Onset usually in patients younger than 50 years. Giant cell arteritis (GCA) Arteritis, often granulomatous, usually affecting the aorta and/or its major branches, with a predilection for the branches of the carotid and vertebral arteries. Often involves the temporal artery. Onset usually in patients older than 50 years and often associated with polymyalgia rheumatica. Medium vessel vasculitis (MVV) Vasculitis predominantly affecting medium arteries defined as the main visceral arteries and their branches. Any size artery may be affected. Inflammatory aneurysms and stenoses are common. Polyarteritis nodosa (PAN) Necrotizing arteritis of medium or small arteries without glomerulonephritis or vasculitis in arterioles, capillaries, or venules, and not associated with antineutrophil cytoplasmic antibodies (ANCAs). Kawasaki disease (KD) Arteritis associated with the mucocutaneous lymph node syndrome and predominantly affecting medium and small arteries. Coronary arteries are often involved. Aorta and large arteries may be involved. Usually occurs in infants and young children. Small vessel vasculitis (SVV) Vasculitis predominantly affecting small vessels, defined as small intraparenchymal arteries, arterioles, capillaries, and venules. Medium arteries and veins may be affected. ANCA‐associated vasculitis (AAV) Necrotizing vasculitis, with few or no immune deposits, predominantly affecting small vessels (i.e., capillaries, venules, arterioles, and small arteries), associated with myeloperoxidase (MPO) ANCA or proteinase 3 (PR3) ANCA. Not all patients have ANCA. Add a prefix indicating ANCA reactivity, e.g., MPO‐ANCA, PR3‐ANCA, ANCA‐negative. Microscopic polyangiitis (MPA) Necrotizing vasculitis, with few or no immune deposits, predominantly affecting small vessels (i.e., capillaries, venules, or arterioles). Necrotizing arteritis involving small and medium arteries may be present. Necrotizing glomerulonephritis is very common. Pulmonary capillaritis often occurs. Granulomatous inflammation is absent. Granulomatosis with polyangiitis (Wegener’s) (GPA) Necrotizing granulomatous inflammation usually involving the upper and lower respiratory tract, and necrotizing vasculitis affecting predominantly small to medium vessels (e.g., capillaries, venules, arterioles, arteries and veins). Necrotizing glomerulonephritis is common. Eosinophilic granulomatosis with polyangiitis (Churg‐Strauss) (EGPA) Eosinophil‐rich and necrotizing granulomatous inflammation often involving the respiratory tract, and necrotizing vasculitis predominantly affecting small to medium vessels, and associated with asthma and eosinophilia. ANCA is more frequent when glomerulonephritis is present. Immune complex vasculitis Vasculitis with moderate to marked vessel wall deposits of immunoglobulin and/or complement components predominantly affecting small vessels (i.e., capillaries, venules, arterioles, and small arteries). Glomerulonephritis is frequent. Anti–glomerular basement membrane (anti‐GBM) disease Vasculitis affecting glomerular capillaries, pulmonary capillaries, or both, with GBM deposition of anti‐GBM autoantibodies. Lung involvement causes pulmonary hemorrhage, and renal involvement causes glomerulonephritis with necrosis and crescents. Cryoglobulinemic vasculitis (CV) Vasculitis with cryoglobulin immune deposits affecting small vessels (predominantly capillaries, venules, or arterioles) and associated with serum cryoglobulins. Skin, glomeruli, and peripheral nerves are often involved. IgA vasculitis (Henoch‐Schönlein) (IgAV) Vasculitis, with IgA1‐dominant immune deposits, affecting small vessels (predominantly capillaries, venules, or arterioles). Often involves skin and gastrointestinal tract, and frequently causes arthritis. Glomerulonephritis indistinguishable from IgA nephropathy may occur. Hypocomplementemic urticarial vasculitis (HUV) (anti‐C1q vasculitis) Vasculitis accompanied by urticaria and hypocomplementemia affecting small vessels (i.e., capillaries, venules, or arterioles), and associated with anti‐C1q antibodies. Glomerulonephritis, arthritis, obstructive pulmonary disease, and ocular inflammation are common. Variable vessel vasculitis (VVV) Vasculitis with no predominant type of vessel involved that can affect vessels of any size (small, medium, and large) and type (arteries, veins, and capillaries). Behçet’s disease (BD) Vasculitis occurring in patients with Behçet’s disease that can affect arteries or veins. Behçet’s disease is characterized by recurrent oral and/or genital aphthous ulcers accompanied by cutaneous, ocular, articular, gastrointestinal, and/or central nervous system inflammatory lesions. Small vessel vasculitis, thromboangiitis, thrombosis, arteritis, and arterial aneurysms may occur. Cogan’s syndrome (CS) Vasculitis occurring in patients with Cogan’s syndrome. Cogan’s syndrome characterized by ocular inflammatory lesions, including interstitial keratitis, uveitis, and episcleritis, and inner ear disease, including sensorineural hearing loss and vestibular dysfunction. Vasculitic manifestations may include arteritis (affecting small, medium, or large arteries), aortitis, aortic aneurysms, and aortic and mitral valvulitis. Single‐organ vasculitis (SOV) Vasculitis in arteries or veins of any size in a single organ that has no features that indicate that it is a limited expression of a systemic vasculitis. The involved organ and vessel type should be included in the name (e.g., cutaneous small vessel vasculitis, testicular arteritis, central nervous system vasculitis). Vasculitis distribution may be unifocal or multifocal (diffuse) within an organ. Some patients originally diagnosed as having SOV will develop additional disease manifestations that warrant redefining the case as one of the systemic vasculitides (e.g., cutaneous arteritis later becoming systemic polyarteritis nodosa, etc.). Vasculitis associated with systemic disease Vasculitis that is associated with and may be secondary to (caused by) a systemic disease. The name (diagnosis) should have a prefix term specifying the systemic disease (e.g., rheumatoid vasculitis, lupus vasculitis, etc.). Vasculitis associated with probable etiology Vasculitis that is associated with a probable specific etiology. The name (diagnosis) should have a prefix term specifying the association (e.g., hydralazine‐associated microscopic polyangiitis, hepatitis B virus–associated vasculitis, hepatitis C virus–associated cryoglobulinemic vasculitis, etc.).
The key to diagnosing a vasculitis is to perform a very complete history including a very detailed review of systems. See Resource (3) below for an example that you can download and print out.
Resources:
(1) 2012 revised International Chapel Hill Consensus Conference Nomenclature of Vasculitides [PubMed Abstract] [Full Text HTML] [Full Text PDF]. Arthritis Rheum. 2013 Jan;65(1):1-11. doi: 10.1002/art.37715.
The above article has been cited by over 100 PubMed articles.
(2) #61: Vasculitis and Giant-Cell Arteritis: ‘Rheum’ for improvement
OCTOBER 9, 2017 By MATTHEW WATTO, MD from The Curbsiders
(3) New Patient Rheumatology History Form (includes a detailed ROS) [Link is to the PDF] From the American College of Rheumatology Accessed 4-13-2019.