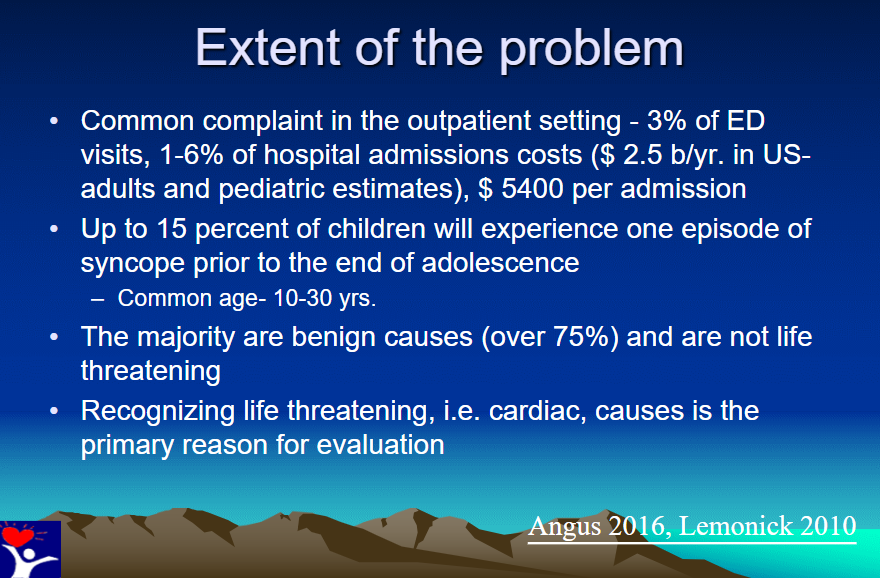
This post contains excerpts from Differentiating Benign From Malignant Syncope by V. Ramesh Iyer MD from the Children’s Hospital of Philadelphia (CHOP). The lecture is from CHOP’s Pediatric Cardiology Course. Dr. Iyer’s lecture was delivered in January of 2018, before the release of the release of the European Society of Cardiology’s 2018 Syncope Guidelines. I’ve included links to those guidelines in Additional Resources after the post.
Two of the keys of determining if the syncope is benign or malignant are the patient’s history and the patient’s family history.
Evaluation in the office or emergency department is covered below and in my post Links To 2018 ESC Guidelines for the diagnosis and management of syncope posted on January 24, 2019 by Tom Wade MD.
If you decide that an extensive evaluation is needed to determine if the syncope is potentially malignant, then the patient may need some or all of the following:
- Careful complete history of the syncopal episode and Past history of any previous syncopal episodes
- Careful family history including any history of SIDS in the family, or death from any cause before 40 years of age.
- Careful physical exam including orthostatic vitals, cardiac auscultation, and neurologic evaluation.
- 12 lead electrocardiogram
- Electrocardiographic monitoring for a time in the office or emergency department
- Longer term arrythmia monitoring following discharge from the care center with either a Holter Monitor or Implantable Loop Recorder.
- Exercise Stress Test
- Complete Echocardiogram
- Cardiac MRI especially if coronary artery anomaly or arrythmogenic right ventricular dysplasia
- Electrophysiology studies
- Evaluation by a geneticist.
Dr. Iyer’s lecture names the causes of life threatening syncope but doesn’t really help primary care clinicians to recognize them. So I’ve done my own post using some of the author’s slides as a scaffold:
Text
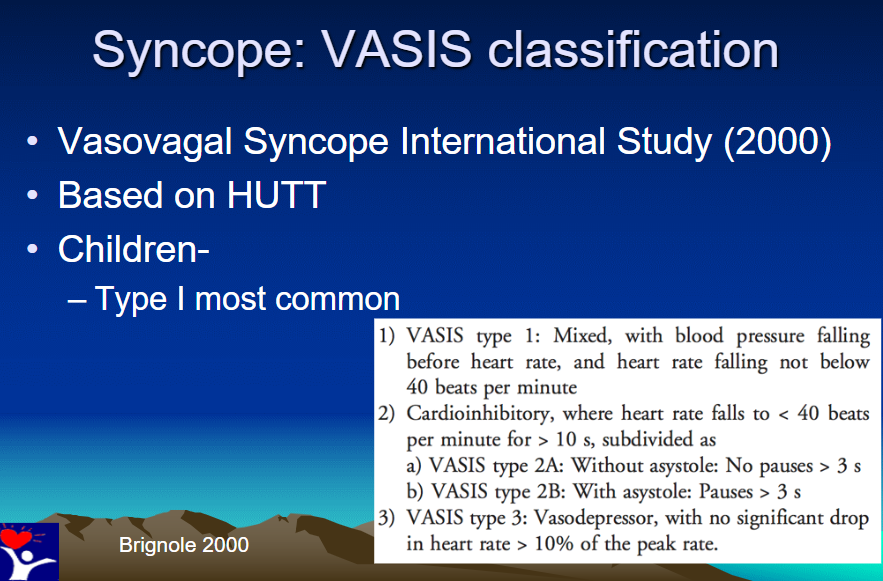
The slide below discusses the the classification of vasovagal syncope:
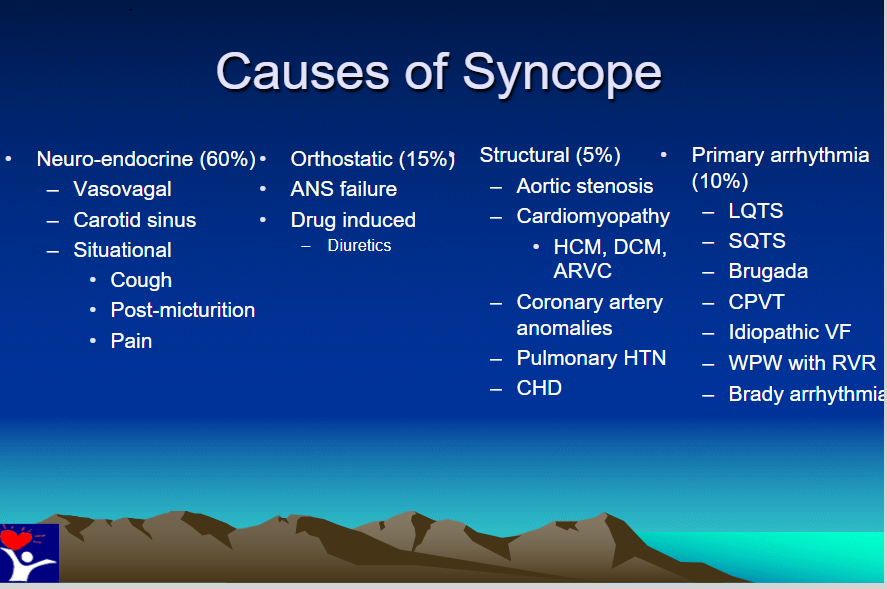
The slide below lists the life-threatening causes of syncope:
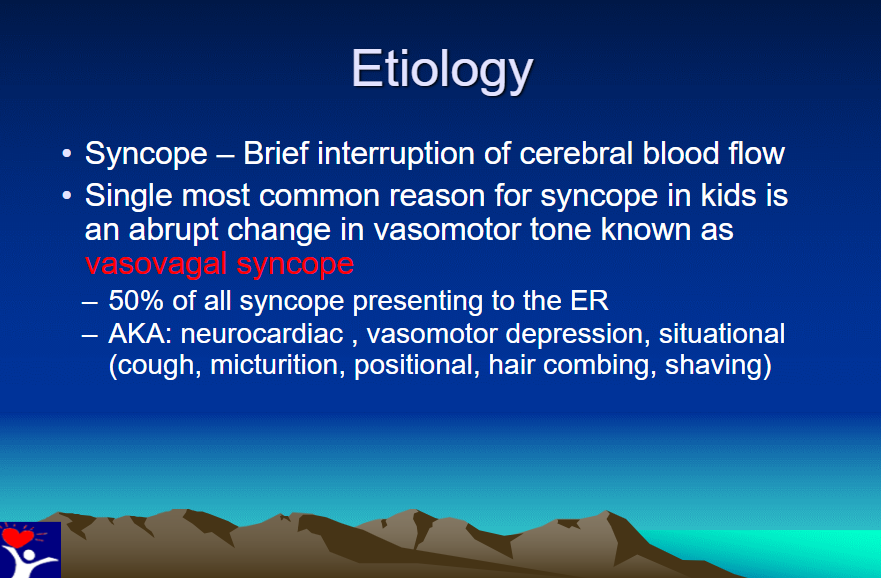
So the first set of causes, neuro-endocrine, account for 60% of syncope and are not life threatening except in certain circumstances (i.e., driving).
The second set of causes, orthostatic hypotension, cause 15% of cases and again are not usually life threatening.
ANS Failure means Autonomic Nervous System Failure.
For information on the diagnosis of ANS Failure see Idiopathic Orthostatic Hypotension and other Autonomic Failure Syndromes Updated: Oct 22, 2018 Author: Mohini Gurme, MD from emedicine.medscape.com. It is an outstanding and brief review of the subject.
The third set of causes of syncope, structural heart disease, cause 5% of syncope. And all of these are life-threatening and need to be detected:
- Aortic Stenosis
- Cardiomyopathy
- Hypertrophic Cardiomyopathy
- Dilated Cardiomyopathy
- Arrythmogenic Right Ventricular Cardiomyopathy
- See Treatment of Arrhythmogenic Right Ventricular Cardiomyopathy/Dysplasia: An International Task Force Consensus Statement 2015 [PubMed Abstract]
- The above article has been cited 21 times in PubMed Central
- See Arrhythmogenic Right Ventricular Dysplasia (ARVD)
Updated: Sep 23, 2014 from emedicine.medscape.com - See Imaging in Arrhythmogenic Right Ventricular Dysplasia (ARVD) Updated: Jun 11, 2018 from emedicine.medscape.com
- See Treatment of Arrhythmogenic Right Ventricular Cardiomyopathy/Dysplasia: An International Task Force Consensus Statement 2015 [PubMed Abstract]
- Coronary Artery Anomalies
- Pulmonary Hypertension
- CHD (Congenital Heart Disease)
The fourth set of causes of life threatening syncope, arrythmias, cause 10% of syncope and are:
- Long QT Syndrome (LQTS)
- See Long QT Syndrome Updated: Nov 29, 2017 from emedicine.medscape.com
- See Pediatric Long QT Syndrome Updated: Jun 26, 2014 from emedicine.medscape.com
- Short QT Syndrome (SQTS)
- Brugada Syndrome
- See Brugada Syndrome Updated: Jan 08, 2017 from from emedicine.medscape.com
- See Paucis Verbis: Brugada syndrome May 6th, 2011 from Academic Life In Emergency Medicine
- Catecholaminergic Polymorphic Ventricular Tachycardia (CPVT)
- Guidelines for the Diagnosis and Management of
Catecholaminergic Polymorphic Ventricular Tachycardia (CPVT) [Full Text PDF] 2016 from The Cardiac Society of Australia and New Zealand - See 2019 Catecholaminergic Polymorphic Ventricular Tachycardia: The Cardiac Arrest Where Epinephrine Is Contraindicated [PubMed Abstract] [Download Full Text PDF]
- See Ohio Student Is Raising Awareness of CPVT SADS Condition 1/15/2019 from SADS (Sudden Arrythmia Death Syndromes Foundation)
- Guidelines for the Diagnosis and Management of
- Idiopathic Ventricular Fibrillation
- Wolf-Parkinson-White Syndrome With Rapid Ventricular Response (WPW with RVR)
- Bradyarrythmia
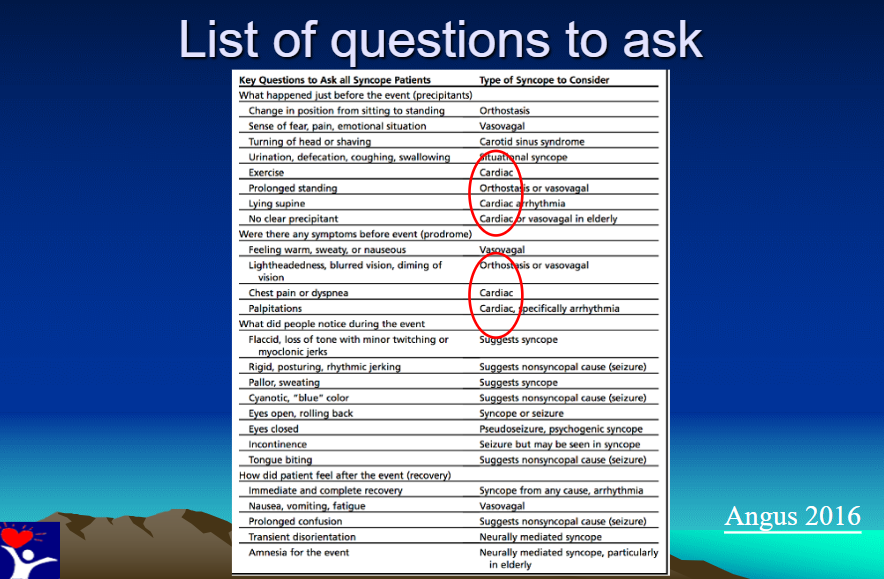
Here is Dr. Iyer’s slide with the questions you should ask the syncope patient:
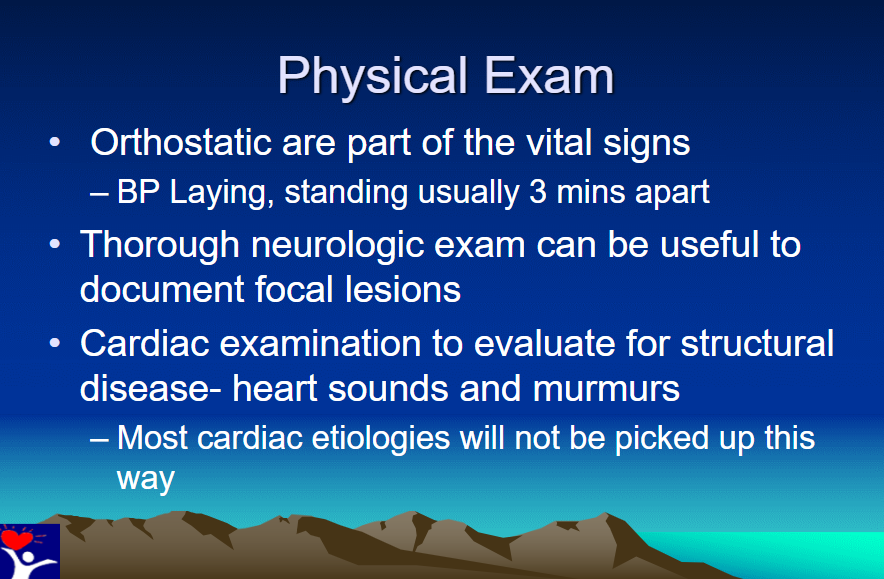
And next is Dr. Iyer’s physical exam:
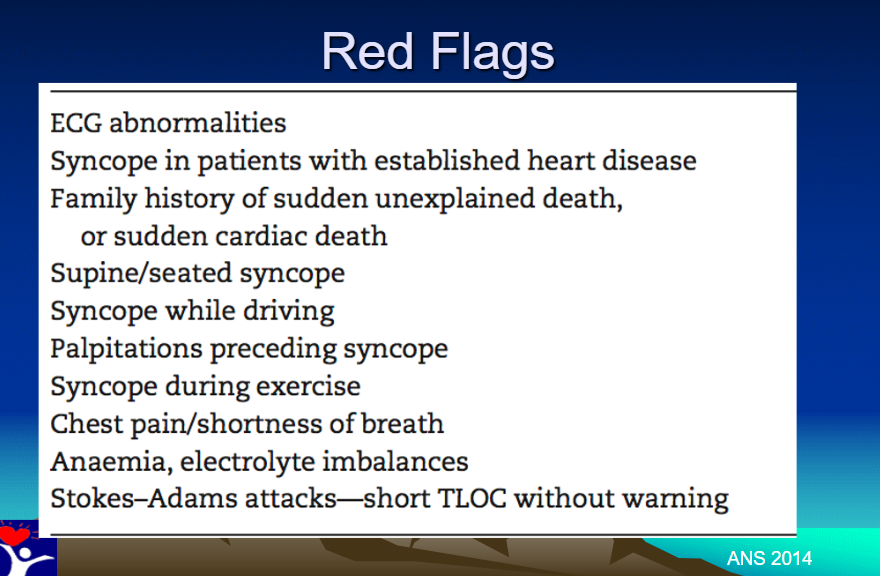
And finally, Dr. Iyer’s Red Flags:
Additional Resources:
(1) 2018 ESC Guidelines for the diagnosis and management of syncope [PubMed Abstract] [Full Text HTML] [Full Text PDF]. Eur Heart J. 2018 Jun 1;39(21):1883-1948. doi: 10.1093/eurheartj/ehy037.
(2) Practical Instructions for the 2018 ESC Guidelines for the diagnosis and management of syncope [Full Text HTML] [Full Text PDF]. European Heart Journal, Volume 39, Issue 21, 1 June 2018, Pages e43–e80.
(3) ‘Ten Commandments’ of ESC Syncope Guidelines 2018: The new European Society of Cardiology (ESC) Clinical Practice Guidelines for the diagnosis and management of syncope were launched 19 March 2018 at EHRA 2018 in Barcelona [Full Text HTML] [Full Text PDF]. European Heart Journal (2018) 39, 1870–1882.