Just listened to and reviewed the podcast and show notes of #80: Pulmonary Hypertension, freeways, and cows in heart failure JANUARY 29, 2018 By MATTHEW WATTO, MD from The Curbsiders.
You should just click on the link above and listen and review. However, I’ve posted the episode here so I’ll have easy access to it via my blog search function. And I’ve also embedded the awesome podcast.
Below, I’ve excerpted some of the show notes from Podcast #80 for my peripheral brain (my personal study notes – meaning this blog).
And I’ve also included in Additional Resources at the end of this post, links to seven other very important resources on the management of pulmonary hypertension.
Resource (1) below after the post contains links to 2015 ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension. It is these guidelines that the Curbsiders #80 podcast is based on.
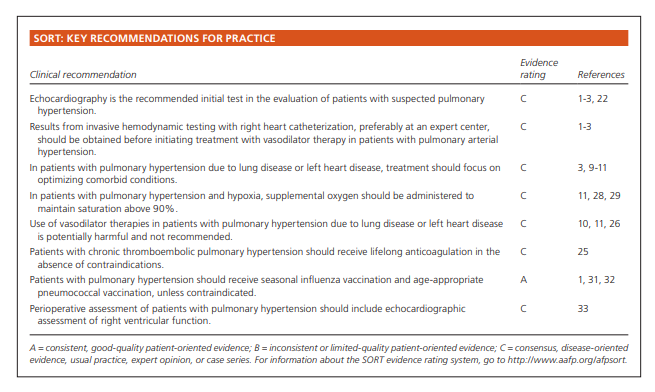
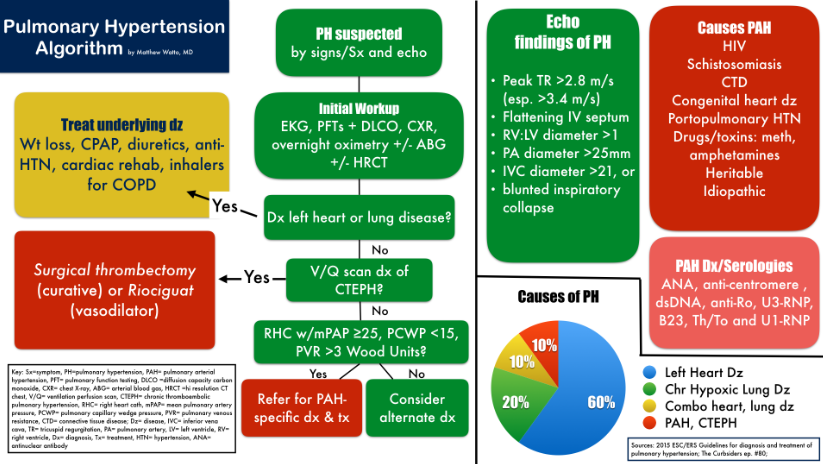
The following chart which nicely summarizes the podcast below and is from an article in American Family Physician. Links to the full article is available in Resource (2) after this post:
In Resource (3) below is an excellent, relatively brief (14 pages) article that contains everything you need to know to use echo to diagnose pulmonary hypertension.
And finally in Additional Resources (4), (5), and (6) below, there are resources that you should review if there is any chance that you will be responsible for the emergency care of patients with pulmonary hypertension. Rapid Sequence Intubation(RSI in a patient) with pulmonary hypertension can lead to cardiac arrest and the these three resources help you manage these fragile patients.
And, frighteningly, many patients with undiagnosed pulmonary hypertension can present to the emergency department and can also arrest during or after RSI.
Resources (4) and (5) below discuss the recognition and management of the above fragile patients (patients with undiagnosed pulmonary hypertension).
And Resource (6) describes a technique for safely (or at least as safely as possible) intubating patients who have or may have pulmonary hypertension.
And Finally, Resource (7) below, Pulmonary Hypertension and Right Ventricular Failure in Emergency Medicine by Dr. Wilcox is an excellent review article.
Now on to the Curbsiders #80:
The clinical information begins at 15:20 of the podcast. All the time before that is entertaining but non-clinical so you can skip it.
See Additional Resources after this post for links to Dr. Scott Weingart’s two outstanding podcasts,
What follows are excerpts from the #80 Curbsiders on Pulmonary Hypertension:
Clinical Pearls
- Pulmonary hypertension (PH) is like a detectable troponin; you must always consider it abnormal and search for an underlying cause.
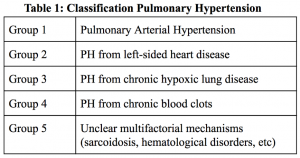
- Ninety percent of PH is due to left heart disease (60%), chronic hypoxic lung disease (20%), or a combination of the two (10%). You must aggressively treat underlying disease and modifiable risk factors.
- Don’t miss chronic thromboembolic pulmonary hypertension (CTEPH)! It’s the ONLY curable cause of PH (via pulmonary endarterectomy). V/Q (ventilation/perfusion) scans are tough to administer & read. Refer to a specialized center if concerned about CTEPH and allow them to perform V/Q scan.
- Pulmonary arterial hypertension (PAH) specific therapies do not cause systemic vasodilation or postural hypotension. Don’t stop PAH-specific therapy, even if blood pressure (BP) is low!! Stopping therapy causes systemic hypotension through increased pulmonary artery pressure (PAP), decreased cardiac output (CO), decreased stroke volume, and a resulting fall in BP.
- Do not use PAH-specific therapies (sildenafil, bosentan, etc.) in PH groups other than Group 1, PAH. These therapies may increase V/Q mismatching and worsen outcomes. The best pulmonary vasodilatory is supplemental oxygen, which should only vasodilate areas being ventilated!
- Prognosis: Life expectancy is 3-5 years w/o treatment. Death is due to right heart failure. Worst prognosis is chronic hypoxic lung disease (group 3) (Gall H, et al. J Heart Lung Transplant. 2017).
See the show notes for Definitions and Classification of Pulmonary Hypertension.
Epidemiology of PH: 90% is due to left heart disease (LHD), chronic hypoxic lung disease, or a combo of the two. The last 10% is due to pulmonary vascular diseases: PAH, CTEPH or rare/miscellaneous causes (i.e. group 5). Breakdown among the 90% is as follows (Strange G et al. Heart. 2012)
- 60%- LHD (systolic/diastolic dysfunction, valvular heart disease, congenital)
- 20%- chronic hypoxic lung disease (COPD, emphysema, pulmonary fibrosis, sleep-disorder breathing, & obesity hypoventilation syndrome)
- 10%- combo of LHD & chronic hypoxic lung disease
And Dr. Ryan reminds us that pulmonary vasodilators such as sildenafil , bosentam, etc are only indicated in pulmonary arterial hypertension. In Left Heart Disease, Chronic Hypoxic Lung Disease, and the Combination of LHD and chronic hypoxic lung disease Sildenafil et all will make the patients worse.
There is, Dr. Ryan states, a specific pulmonary vasodilator for chronic hypoxic lung disease and it is oxygen and the treatment of sleep disordered breathing if present.
Diagnosis
- Questions to ask: Can you walk as far as you want? How far can you walk? Can you walk “on the flats” without shortness of breath? When were you last 100%? Have you had syncope? Angina? *Presence of syncope or angina indicate a poor prognosis.
- Initial Workup (2015 European Guidelines): Echo, 6-Minute walk test, NYHA functional class, EKG, pulmonary function testing (PFTs) including spirometry & DLCO, chest xray, overnight oximetry, and arterial blood gas (room air) if concern for obesity hypoventilation syndrome. Hi-res CT chest can be considered in select patients.
- Echocardiogram: Measures right ventricular systolic pressure (RVSP), which is an estimate of pulmonary artery systolic pressure (PASP). Accurate to within 10-15 mmHg. Normal RVSP = 20-24 mmHg. An elevated RVSP = >35 mmHg [correlates with a PA diastolic pressure of 10-15 & mean PAP of ~25 mmHg]
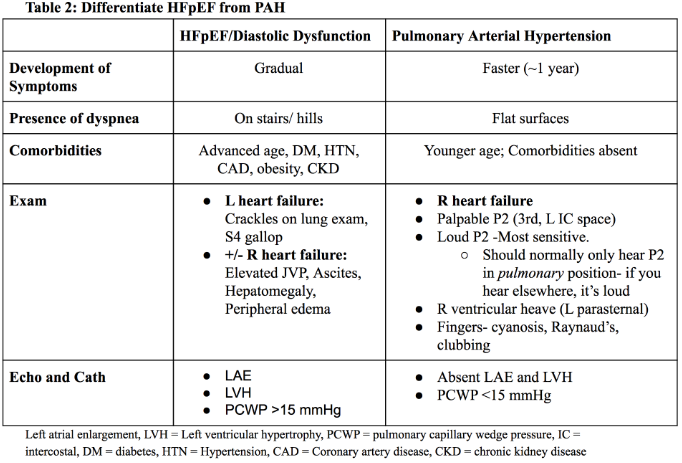
- Echo findings in LHD: Presence of L atrial enlargement, L ventricular hypertrophy provide 94% confidence that PH is from left heart disease (Thenappan T et al. Circ Heart Fail 2011).
- Differentiating types of PH: “Look at the company it keeps” (e.g. A patient w/obesity, HTN, CAD, and diabetes more likely to have LHD; If lupus or scleroderma present then more likely PAH). Combine the history, exam, and echo findings to accurately predict etiology. (see table 2 for PAH vs. heart failure with preserved ejection fraction [HFpEF]
Diagnosis (continued)
- CTEPH suspected?: Check *V/Q scan (+/- CT pulmonary angiogram). *Dr Ryan suggests this be done at a center specializing in PH.
- PAH risk factors: HIV, schistosomiasis, congenital heart disease, portopulmonary HTN, connective tissue disease (lupus, scleroderma, mixed CTD), drugs/toxins (listed in #10), heritable (source 2015 ESC/ERS g/l)
- PAH suspected?: Check HIV; hepatitis; schistosomiasis serology (returning travelers); connective tissue disease (CTD) panel, see below; screen for drugs/toxins (see list below); hereditary conditions
- CTD panel: Antinuclear antibodies: anti-centromere, dsDNA, anti-Ro, U3-RNP, B23, Th/To and U1-RNP. Tests lupus, scleroderma, and mixed connective tissue disease.
- Drugs-Toxins implicated in PAH: Definite– fenfluramine, SSRIs (maternal use affecting newborn);Likely– amphetamine, methamphetamine; Possible– cocaine, St John’s Wort, interferon, certain alkylating chemotherapeutic agents (e.g. cyclophosphamide)
Treatment
- PH from chronic heart and lung disease (groups 2, 3): TREAT UNDERLYING CAUSE! Modify risk factors. Encourage weight loss. Ensure compliance with CPAP. Ask about chronic angina, and if present refer for cardiac rehab. Trial diuretics. Treat hypertension.
- Diuretic therapy: Dr Ryan finds combination of loop diuretic (e.g. furosemide) and potassium sparing diuretic (e.g. spironolactone, amiloride) are effective and well tolerated to control hypertension and optimal volume status. Utilize ACE inhibitor if further BP control needed.
- Follow up after Tx initiated: At 12 weeks consider repeating echo, NYHA functional class assessment, 6-Minute walk test. Consider a right heart cath (RHC) if not improving.
- When to refer: Syncope; NYHA functional class III or IV; atypical presentation; workup fails to identify a cause; patient w/PAH risk factors (see #14); congenital heart disease; suspicion of CTEPH; You feel confused or uncomfortable : )
Additional Resources:
(1) 2015 ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension: The Joint Task Force for the Diagnosis and Treatment of Pulmonary Hypertension of the European Society of Cardiology (ESC) and the European Respiratory Society (ERS): Endorsed by: Association for European Paediatric and Congenital Cardiology (AEPC), International Society for Heart and Lung Transplantation (ISHLT) [PubMed Abstract] [Full Text HTML] [Full Text PDF]. Eur Heart J. 2016 Jan 1;37(1):67-119. doi: 10.1093/eurheartj/ehv317. Epub 2015 Aug 29.
(2) Pulmonary Hypertension: Diagnosis and Treatment [Full Text HTML] [Full Text PDF]. Am Fam Physician. 2016 Sep 15;94(6):463-469.
(3) Echocardiography in Pulmonary Arterial Hypertension: from Diagnosis to Prognosis [PubMed Abstract] [Full Text HTML] [Full Text PDF]. J Am Soc Echocardiogr. 2013 Jan;26(1):1-14. doi: 10.1016/j.echo.2012.10.009. Epub 2012 Nov 8.
(4) Emergency Recognition And Management Of Pulmonary Hypertension And RV Failure – Help From Drs. Wilcox and Weingart (EMCrit 181)
Posted on July 25, 2018 by Tom Wade MD
(5) Podcast 181 – Pulmonary Hypertension and Right Ventricular Failure with Susan Wilcox September 5, 2016 by Dr. Scott Weingart.
(6) EMCrit RACC Podcast 216 – The Hemodynamically Neutral Intubation
January 22, 2018 by Dr. Scott Weingart
(7) Pulmonary Hypertension and Right Ventricular Failure in Emergency Medicine [PubMed Abstract] [Full Text PDF]. Ann Emerg Med. 2015 Dec;66(6):619-28. doi: 10.1016/j.annemergmed.2015.07.525. Epub 2015 Sep 3.