In this post, I link to three resources I have reviewed and recommend for the evaluation of pediatric limp.
A Systematic Approach to the Evaluation of a Limping Child [PubMed Abstract] [Full-Text HTML] [Full-Text PDF]. Am Fam Physician. 2015 Nov 15;92(10):908-16.
Abstract
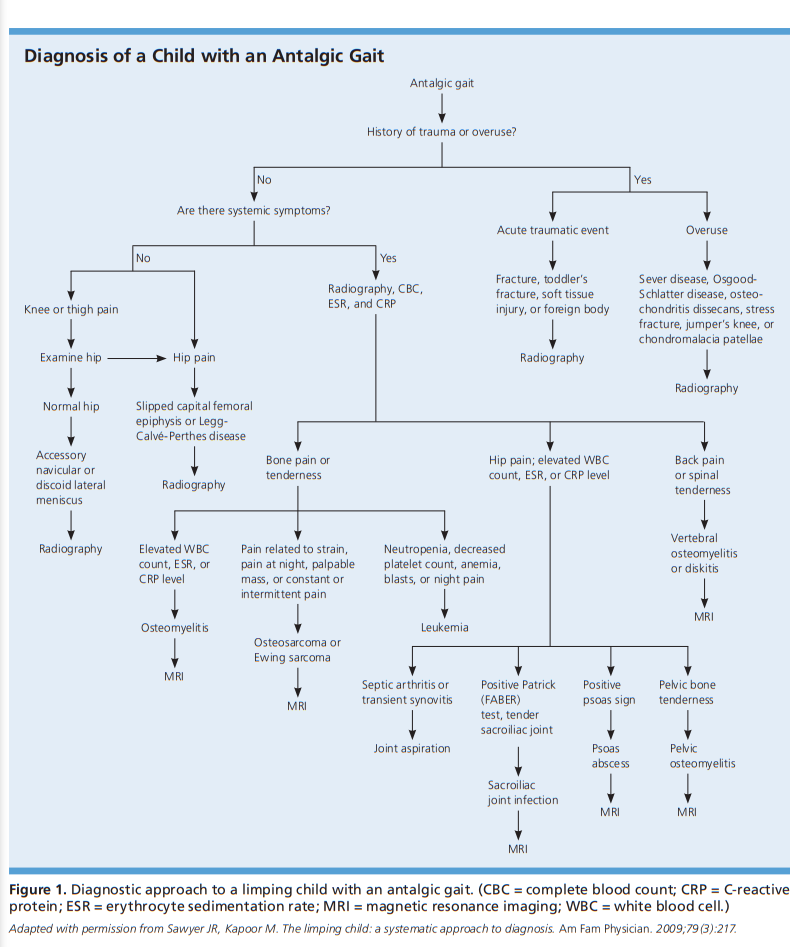
A limp is defined as a deviation from a normal age-appropriate gait pattern resulting in an uneven, jerky, or laborious gait. It can be caused by pain, weakness, or deformity as a result of a variety of conditions. Transient synovitis is the most common diagnosis. Other causes of acute limp include contusion, foreign body in the foot, fracture, osteomyelitis, septic arthritis, reactive arthritis, and Lyme arthritis. Causes of chronic limp include rheumatic disease, dermatomyositis, acute rheumatic fever, inflammatory bowel disease, and systemic lupus erythematosus. Evaluation of a limping child should begin with a history focused on identifying pain, trauma, and associated systemic symptoms. For a limping child with focal findings on physical examination, initial imaging includes anteroposterior and lateral radiography of the involved site. If there are no focal findings on physical examination, radiography of both lower extremities should be performed. Laboratory testing is guided by history and physical examination findings. Septic arthritis of the hip should be suspected in a child with an oral temperature more than 101.3°F (38.5°C), refusal to bear weight, erythrocyte sedimentation rate more than 40 mm per hour, peripheral white blood cell count more than 12,000 per mm3 (12 × 109 per L), or C-reactive protein level more than 20 mg per L (180.96 nmol per L).
Transient Synovitis or Septic Arthritis? Evaluating the Kocher Criteria
September 24, 2018, from Taming the SRU: Emergency Medicine Tamed
When a child presents with atraumatic hip pain, the differential includes septic arthritis, transient synovitis, osteomyelitis, slipped capital femoral epiphysis, Legg- Calve-Perthes disease, juvenile idiopathic arthritis, acute rheumatic fever, post strep reactive arthritis, gonococcal arthritis, Henoch-Schoenlein purpura, sickle cell crisis, lyme arthritis, etc. The list is extensive. Fortunately, many of these complaints can be ruled out using a good history, physical exam, and basic laboratory/imaging tests. Two diagnoses, however, are notoriously hard to differentiate without an invasive procedure: septic arthritis and transient synovitis. Both present with an atraumatic, acutely irritable hip sometimes with associated limp, fever, refusal to bear weight, limited ROM, and/or joint effusion on x-ray and ultrasound. It is imperative to differentiate the two as the treatment and course of the two diseases are very different.
WHAT DOES ALL THIS MEAN?
Investigators at many different institutions have not been able to agree on which criteria are the most predictive of a septic joint. There has yet to be a high quality and affirmative external validation of the Kocher Criteria. The positive predictive value of the Kocher criteria depends on the prevalence of disease with lower positive predictive value with lower prevalence of disease. Most importantly, absence of all 5 criteria (Kocher Criteria + CRP) confers a very low probability of having septic arthritis.
SUMMARY
A detailed history and physical exam are critical in the assessment of pediatric hip pain. Subsequent investigations including laboratory and imaging studies should be guided by your pre-test probability of septic arthritis. The Kocher criteria, especially when used in conjunction with CRP, can help guide the need for arthrocentesis and consultation of orthopedic surgery however the positive predictive value of the criteria is variable.
Ultimately, a patient with 0 of 4 Kocher criteria, a negative CRP, and a low pre-test probability of septic arthritis can reasonably be managed as an outpatient with NSAIDS and strict return precautions for worsening hip pain and/or fever. Increasing uncertainty, either by history and/or the presence of Kocher criteria, mandates the need for further investigation with arthrocentesis and/or consultation with orthopedics as misdiagnosis of septic arthritis can have dire consequences.
The limping or non-weight bearing child, Clinical Practice Guidelines from The Royal Children’s Hospital Melbourne. Last updated, July 2020.
See also
Fractures
Bone and joint infections
Acutely swollen joint
Child abuseKey points
- Most children presenting with a limp do not require investigations
- Observing the child’s gait may help localise the problem and narrow the differential diagnosis
- Acute inability to walk or weight-bear is a red flag
- Septic arthritis is an orthopaedic emergency and should be considered in all limping children with severe localised joint pain and fever
Background
- Transient synovitis, acute myositis and minor trauma are common causes of limp in children, but serious pathology should be excluded
- Pain causing limp can be referred. Therefore, a thorough assessment of joints above and below (including the spine and other relevant body systems) is essential to accurately localise the source
Assessment – Review the extensive Data in the Guideline
Management
Investigations
- No investigations are indicated if all of the following apply:
- no red flags in the history and physical examination
- ambulating with mild or no discomfort with simple analgesia
- a clear working diagnosis and/or a plan for review within 7 days of onset of limp
- Imaging
- X-ray (area of suspicion)
- pelvis AP or frog leg view is useful for identifying SUFE, DDH (>6 mo), Perthes disease and common pelvic avulsions
- normal x-ray does not exclude septic arthritis or early osteomyelitis
- Ultrasound (hip)
- assess for presence of drainable effusion when septic arthritis is suspected
- presence of an effusion often does not differentiate between septic arthritis and transient hip synovitis
- Other eg bone scan or localised MRI if still limping at 7 days, consult local paediatric, orthopaedic or radiology services
- Laboratory
- Raised inflammatory markers (platelets, WCC, CRP +/- ESR) may suggest infective or inflammatory picture. These may be normal in contained or chronic infections
- Blood cultures (pre-antibiotics if possible) if osteomyelitis, septic arthritis or septic bursitis are suspected
- FBE and film if any concern for haematological malignancy
Consider consultation with local paediatric team when
- There is possible non-accidental injury
- There are clinical or laboratory features of malignancy
- Systemically unwell
- Symptoms last more than 7 days, or child unable to weight-bear or permit movement after analgesia
- Suspecting septic arthritis – consult with orthopaedic team
Consider transfer when
Child requires care above the level of comfort of the local hospital
For emergency advice and paediatric or neonatal ICU transfers, see Retrieval Services
Consider discharge when
- The cause of the limp has been identified and adequately managed
OR- Child is ambulating comfortably with or without analgesia AND
- High risk diagnoses have been considered AND
- Adequate follow up plan in place